1601006065 case presentation
LONG CASE
A 55 Yr old female ,housewife, resident of Guntur (macharla) informant being daughter presented with chief complaints of
-Weakness of Upper limb since 1 day (afternoon)
-Weakness of right Lower limb since 1 day
-Inability to speak since night
-Confusion at the time of admission
HOPI:
Patient was apparently normal 2 days back later on, primarily she developed giddiness in the morning which later resolved on next day by medication prescribed by RMP (CINARIZINE)
On examination by RMP ,he also found that her sBP was around 280 mmhg and gave antihypertensive (TELMISARTAN)
On the next day,while she was going to washroom she was unable to lift her right hand and move her right leg ,unable to do her daily routine
She was dragging her leg which was noticed by her daughter and later on was laid down to bed and at the night she was unable to lift herself up to use the washroom ,so she was brought to hospital
On the way to hospital, she was unable to recognize her daughter's and unable to speak .
Past history:
For Diabetes -T. Dapaglifozin 10mg, T. Metformin 500mg
For Hypertension :T.Telma 40 mg T.Cilindipine 10mg T.Metoprolol 50mg
Personal History: Diet Mixed
Appetite normal
Bowel And Bladder
Sleep Adequate
No Allergies And Addictions.
Family History : not Significant
General Examination:
Patient is Conscious, but not Cooperative and is oriented to Place and Person.
Moderately Built and Nourished.
No signs of Pallor,Icterus ,Clubbing, Cyanosis,Lymphadenopathy
Vitals :
Temp - 100.8F
PR- 90 bpm
B.P -180/80mmHg
SpO2 94%.
SYSTEMIC EXAMINATION :
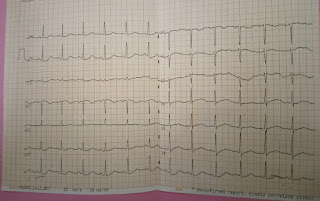
CVS : S1 S2 heard, no murmurs
RS : Bilateral air entry present, normal vesicular breath sounds, no added sounds
GIT : Soft, non-tender, no organomegaly
Higher Mental Functions
Right handed individual
Patient level of consciousness -E4 V1 M4
Higher mental functions are intact
Speech - Markedly reduced , Not assessable
Signs of meningeal irritation ( neck stiffness,kernigs sign )are absent
Cranial nerves -
Upper limb. R. L
TONE Hypotonic N
POWER
DELTOID. 2+. 4+
BICEPS. 2+. 5+
TRICEPS. 2+. 5+
Lumbricals. 2+. 5+
REFLEXES
B +. ++
T. +. ++
S. +. ++
lower limbs. R. L
TONE. Hypotonic. Normal
POWER
EXTENSORS OF HIP. 2+. 2+
FLEXORS OF KNEE 2+. 2+
EXTENSORS OF KNEE. 2+. 2+
PLANTAR FLEXION 2+. 2+
DORSI FLEXION. 2+. 2+
REFLEXES
CORNEAL present. Present
CONJUNCTIVAL present. Present
KNEE JERK. + 2+
ANKLE JERK + 2+
PLANTAR. Extensor Flexor
A 52 yr male came with chief complaints of reddish erythematous plaque over both lower limbs with itching and dryness over them since 2 and half years
HOPI:
Pt was apparently normal two and half years back ,then starting suffering from reddish erythematous plaque overboth lower limbs with itching and dryness over them ,he took medication for above complaints but there was no satisfactory relief, so he came to our hospital for further treatment
PAST HISTORY:
K/C/o HTN since 8 years and is on regular medication (TELMA 40)
Not a k/c/o DM,EPILEPSY,ASTHMA,TB,CAD,CVA
PERSONAL HISTORY:
Diet -Mixed
Appetite -normal
Decreased sleep due to itching
Bowel And Bladder-regular and normal
No addictions
FAMILY HISTORY:
No family History of any dermatological disorders
General Examination:
On examination pt is conscious,coherent,cooperative
Moderately built
No signs of pallor,icterus cyanosis,clubbing,generalisedlymphadenopathy, pedal edema
Systemic Examination
CVS-S1 S2 heard No murmurs
RS-BAE present,NVBS heard
Per Abdomen-soft,non tender ,bowel sounds heard
CNS- no focal neurological deficit
Local Examination:
Red scaly palpules and plaques noted over the rt palm,rt and left leg,rt foot
GRATTAGE TEST POSITIVE




















Comments
Post a Comment