1701006006 CASE PRESENTATION
LONG CASE
51 year old male patent resident of Suryapet and he works in Goods transportation company came to the hospital with
CHEIF COMPLAINS of
Fever since 10 days
Cough since 10 days
shortness of breath since 6 days
HISTORY OF PRESENTING ILLNESS
FEVER
since 10 days which is high grade
ASSOCIATED with chills and rigors intermittent
RELIVED with medication.
Associated with cough and shortness of breath.
NOT ASSOCIATED with night sweats
COUGH
since 10 days which is productive ,
mucoid in consistency,
whitish ,scanty amount ,
more during night times
AGGREVATED on supine position
non foulsmelling ,
non bloodstained .
RIGHT SIDED PAIN
diffuse , intermittent ,dragging type ,
AGGREVATED ON cough ,
NOT ASSOCIATED with sweating , palpitations.
No history of pain associated with movement
SHORTNESS OF BREATH
since 6 days , insidious onset
gradually progresive
grade 3 (MMRC)
NOT ASSOCIATED with wheeze ,no orthopnea ,no Paroxysmal nocturnal dyspnea, no pedal edema .
No history of weight loss ,no loss of appetite
No history of pain abdomen or abdominal distension , vomitings ,loose stools .
No history of burning micturition.
PAST HISTORY
Patient gives history jaundice 15 days back that resolved in a week .
No history of Diabetes , Hypertension , Tuberculosis ,Bronchial asthma ,COPD , coronary artery disease , Cerebrovascular accident ,thyroid disease.
Family history :
No similar illness in the family
Personal history :
Patient is a chronic smoker - smokes 5 cigarettes per day from past 25 years .
He is a Chronic alcoholic -
cosumes 300 ml whisky per day ,
NO ALCOHOL INTAKE since 3 months.
bowel and bladder regular
differentials -Pneumonia ??Pleural effusion ??
GENERAL EXAMINATION :
Patient is moderately built and nourished.
He is conscious, comfortable.
No signs of
pallor
cyanosis ,
Clubbing,
icterus ,
koilonychia ,
lymphadenopathy
Edema
VITALS
Patient is afebrile .
Pulse - 86 beats / min ,normal voulme ,regular rhythm,normal character ,no radiofemoral delay.
BP - 110/70 mmhg ,measured in supine position in both arms .
Respiratory rate -22 breaths / min
SYSTEMIC EXAMINATION :
Patient examined in sitting position
Inspection:-
oral cavity- Nicotine staining seen on teeth and gums ,nose,chest movements NORMAL
Respiratory movements appear to be decreased on right Side
Trachea is central in position & Nipples are in 4th Intercoastal space
Apex impulse visible in 5th intercostal space
Palpation:-
All inspiratory findings are confirmed
Trachea central in position
Apical impulse in left 5th ICS,
1cm medial to mid clavicular line
Respiratory movements decreased on right side
Tactile and vocal fremitus reduced on right side in infra axillary and infra scapular region
PERCUSSION
DULL NOTE IN RIGHT SIDE IN
Mammary
axillary
infra axillary
Inter-scapular
intra scapular
AUSCULTATION DECREASED ON RIGHT SIDE in above areas
Gastrointestinal system :
Inspection -
-Abdomen DISTENDED
-All quadrants of abdomen are equally moving with respiration except Right upper quadrant
No visibe sinuses ,scars , visible pulsations or visible peristalsis
Palpation:
All inspectory findings are confirmed.
No tenderness .
Liver - is palpable 4 cm below the costal margin and moving with respiration.
Spleen : not palpable.
Kidneys - bimanually palpable.
Percussion - normal
Traubes space
Auscultation- bowel sounds heard .
No bruits .
Cardiovascular system -
S1 and S 2 heard in all areas ,no murmurs
Final Diagnosis :
Right sided Pleural effusion likely infectious etiology.
Investigations :
Pleural fluid analysis :
Colour - straw coloured
Total count -2250 cells
Differential count -60% Lymphocyte ,40% Neutrophils
No malignant cells.
Pleural fluid sugar = 128 mg/dl
Pleural fluid protein / serum protein= 5.1/7 = 0.7
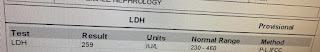
Pleural fluid LDH / serum LDH = 0.6
Interpretation: Exudative pleural effusion.
Serology negative
Serum creatinine-0.8 mg/dl
CUE - normal
CT abdomen
Final Diagnosis:
1-Right sided Pleural effusion - synpneumonic effusion
2- Liver Abscess .








































Comments
Post a Comment