1701006008 CASE PRESENTATION
LONG CASE
A 50 year old male patient who is a farmer and a daily wage worker by occupation, a resident of Pochampally, came to the general medicine department on 02-06-2022 with
CHIEF COMPLAINTS :
There is no local rise of temperature.
No hepatomegaly. No splenomegaly.
Guarding is present.
Rigidity is absent.
Kidney not palpable.
Shifting dullness : Positive
Fluid thrill : Positive
Liver span could not be detected.
No renal angle tenderness.
Auscultation :
Bowel sounds are decreased.
No bruits could be heard.
Cardiovascular System : S1, S2 heard
Respiratory System : Normal vesicular breath sounds heard
Central Nervous System : Conscious; Speech normal ; Motor and sensory system examination is normal, Gait is normal.
INVESTIGATIONS :
1. Hemogram :
Hemoglobin : 9.8 g/dl
TLC : 7,200
Neutrophils : 49%
Lymphocytes : 40%
Eosinophils : 1%
Basophils : 0%
PCV : 27.4%
MCV : 92.3 fl
MCH : 33 pg
MCHC : 35.8%
RDW-CV : 17.6%
RDW-SD : 57.8 fl
RBC count : 2.97 millions/mm3
Platelet count : 1.5 lakhs/mm3
Smear : Normocytic normochromic anemia
2. Serology :
HbsAg : Negative
HIV : Negative
3. ESR :
15mm/1st hour
4. Prothrombin time : 16 sec
5. APTT : 32 sec
6. Serum electrolytes :
Sodium : 133 mEq/L
Potassium : 3 mEq/L
Chloride : 94 mEq/L
7. Blood Urea : 12 mg/dl
8. Serum Creatinine : 0.8 mg/dl
9. LFTs :
Total Bilirubin : 2.22 mg/dl
Direct Bilirubin : 1.13 mg/dl
AST : 147 IU/L
ALT : 48 IU/L
ALP : 204 IU/L
Total proteins : 6.3 g/dl
Serum albumin : 3 g/dl
A/G ratio : 0.9
10. Ascitic fluid :
Protein : 0.6 g/dl
Albumin : 0.34 g/dl
Sugar : 95 mg/dl
LDH : 29.3 IU/L
SAAG : 2.66 g/dl
11. Ascitic Fluid Cytology :
12. Ascitic fluid culture and sensitivity report :
13. Ultrasound :
Coarse echotexture and irregular surface of liver - Chronic liver disease
Gross ascites
Gallbladder sludge
14. ECG
15. X-ray
PROVISIONAL DIAGNOSIS :
Decompensated Chronic liver disease with ascites most likely etiology is alcohol.
TREATMENT :
Drugs :
1. Inj. Pantoprazole 40 mg IV OD
2. Inj. Lasix 40 my IV BD
3. Inj. Thiamine 1 Amp in 100 ml IV TID
4. Tab. Spironolactone 50 mg BB
5. Syrup Lactulose 15 ml HS
6. Syrup Potchlor 10ml PO TID
7. Fluid restriction less than 1L/day
8. Salt restriction less than 2g/day
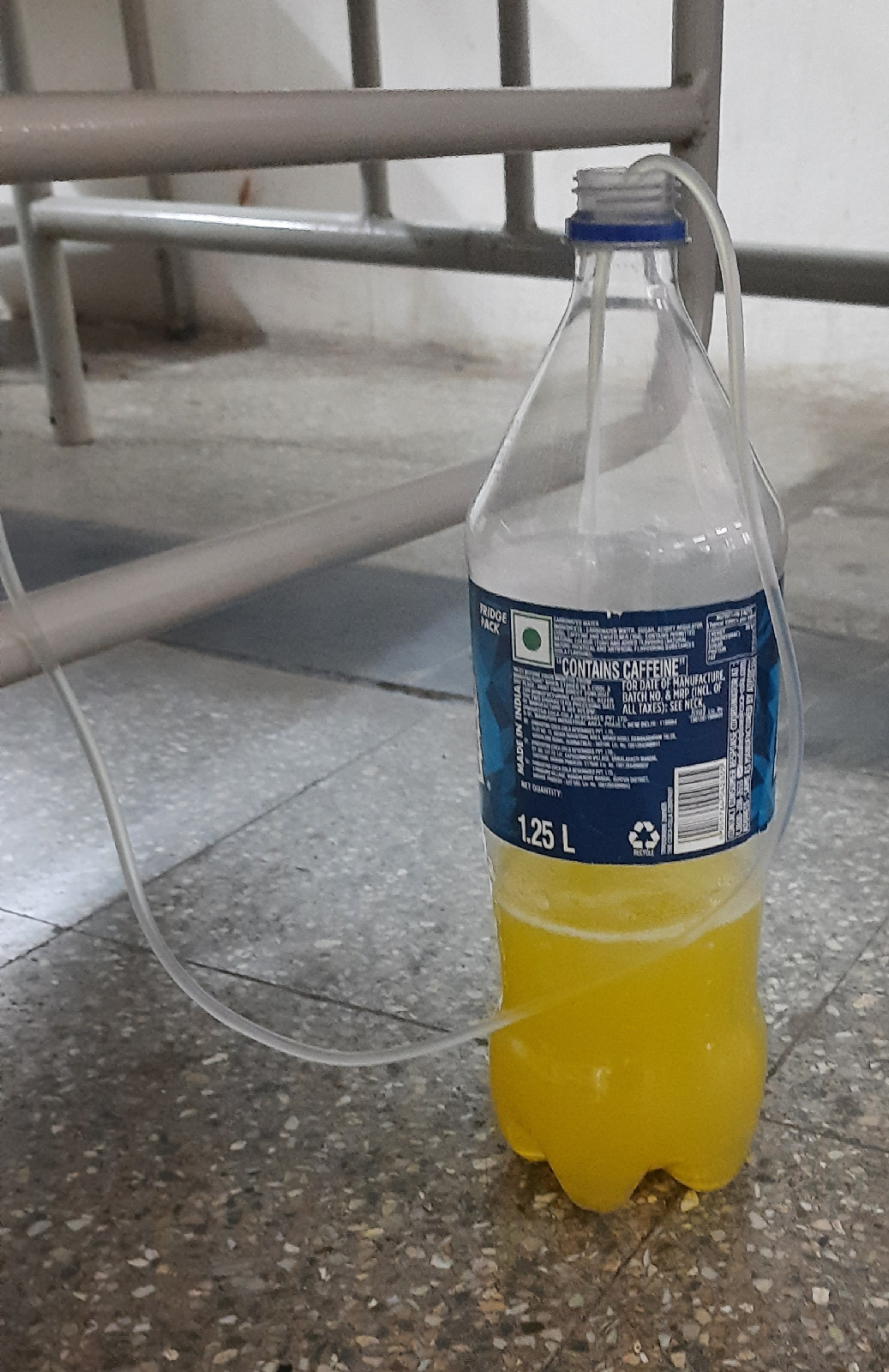
Ascitic fluid tapping :
Ascitic fluid was tapped twice (2-06-2022 and 6-06-2022)
A 56 year old male patient, daily wage worker by occupation, resident of Nalgonda came to opd on 28-05-22 with
CHIEF COMPLAINTS :
1. Pain abdomen since 20 days.
2. Multiple abdominal swellings since 7 days.
3. Fever since 7 days
HISTORY OF PRESENT ILLNESS :
Patient was apparently asymptomatic 5 months back, then he developed cough which was insidious in onset, gradually progressive and there was no sputum. Later, he developed fever which was high grade, associated with chills and rigors. He went to the hospital with above complaints and medications were prescribed and the symptoms subsided.
After 2 months, patient observed loss of appetite and loss of weight for which he went to the doctor. Upon, his advice, the patient got tested for Tuberculosis and HIV. He tested positive for both TB and HIV. The patient was given ART and ATT.
20 days back, patient started experiencing pain around the umbilicus which was insidious in onset, gradually progressive associated with abdominal discomfort. He complains of small multiple round swellings in the abdomen since 7 days which have gradually increased to present size. He had fever since 7 days which was high grade associated with chills and rigors.
PAST HISTORY :
Patient is a known case of Tuberculosis and HIV-AIDS and is on regular treatment.
Patient is not a known case of Diabetes mellitus, Hypertension, Asthma, Epilepsy, Thyroid disorders.
There is no surgical history, no history of blood transfusions.
PERSONAL HISTORY :
Diet : Mixed
Appetite : Decreased
Sleep : Adequate
Bowel and Bladder movements : Regular
Addictions : None
FAMILY HISTORY :
No history of similar complaints in the family.
HISTORY OF ALLERGIES :
No known drug or food allergies.
GENERAL PHYSICAL EXAMINATION :
Patient is conscious, coherent, co-operative and well oriented to time, place and person.
Moderately built and moderately nourished.
No pallor, icterus, cyanosis, clubbing, edema
Lymphadenopathy is present. There are multiple enlarged lymph nodes in abdomen and neck.
Cervical lymph nodes : Palpable on both sides of neck which are about 2x2 cm in size and soft to firm in consistency.
palpation of cervical lymph nodes
Inguinal lymph nodes : Multiple palpable lymph nodes on both sides of size about 1x1 cm which are soft to firm in consistency are palpable.
Axillary and supraclavicular lymph nodes are not palpable.
Vitals :
Temperature : Febrile
Pulse Rate : 86 bpm
Blood Pressure : 120/80 mm Hg
Respiratory rate : 16 cpm
GRBS : 106 mg/dl
SYSTEMIC EXAMINATION :
Cardiovascular System : S1, S2 heard. No murmurs.
Respiratory System : Normal Vesicular Breath Sounds heard.
Central Nervous System : Conscious, Alert, Speech normal, Motor and Sensory examination normal.
Per Abdomen : Soft. No hepatomegaly. No splenomegaly.
INVESTIGATIONS :
1. Hemogram
Hemoglobin : 7.3 g/dl
TLC : 4000 cells/mm3
Neutrophils : 78%
Lymphocytes : 13%
Eosinophils : 2%
Basophils : 0%
PCV : 20.7 vol%
MCV : 85.2 fl
MCH : 30 pg
MCHC : 35.3%
RDW-CV : 17.2%
RDW-SD : 53.7 fl
RBC count : 2.43 million/mm3
Platelet count : 2.61 lakhs/mm3
Smear : Normocytic Normochromic anemia
2. Blood sugar :
97 mg/dl
3. ESR : 45 mm/1st hour
4. CRP : Positive (2.4 mg/dl)
5. LDH : 261 IU/L
6. HIV : Reactive
7. LFT :
Total Bilirubin : 1.22 mg/dl
Direct Bilirubin : 0.24 mg/dl
AST : 43 IU/L
ALT : 22IU/L
ALP: 375IU/L
Total protein : 6.4 g/dl
Albumin : 3g/dl
A/G : 0.88
8. RFT :
Urea : 20 mg/dl
Creatinine : 0.8 mg/dl
Uric acid : 4.0 mg/dl
Calcium : 9.3 mg/dl
Phosphorus : 3.3 mg/dl
Sodium : 139 mEq/L
Potassium : 4.1 mEq/L
Chloride : 102 mEq/L
9. CUE
10. ECG
11. Chest x-ray
12. 2D Echo
PROVISIONAL DIAGNOSIS :
Fever with generalized lymphadenopathy secondary to HIV/TB
TREATMENT :
1. Tab. Dolo 650 PO TID
2. Tab. MVT OD
3. Inj. Neomol 1g IV/SOS
4. Tab. Dolutegravir, Lamivudine, Tenofovir Disoproxil Funerate (50 mg,300 mg,300 mg) PO OD
5. Tab. Rifampicin, Isoniazid, Pyrazinamide, Ethambutol (150 mg,75 mg,400 mg,275 mg) PO OD
6. Tab. Septran-DS PO BD
7. Tab. Pan 40 mg PO BD
8. Syrup Aristozyme PO 10 ml TID




























Comments
Post a Comment