1701006016 CASE PRESENTATION
LONG CASE
A 70 year old male, who is a daily wage worker came with the
CHIEF COMPLAINTS:
1- Breathlessness (since 20 days)
2-Cough( since 20 days)
3-Fever(since 4 days)
HISTORY OF PRESENTING ILLNESS :
Patient was apparently asymptomatic 20 days back,then he developed
Breathlessness- MMRC - Grade -2 and 3 aggrevated on exertion and on exposure to cold,associated with wheeze no orthopnea and no PND. Relieved on rest.
Cough with expoctoration - mucoid,non foul smelling and non blood stained, increased during night, no postural and diurnal variations relieved on taking medication.
fever,low grade evening rise of temperature,not associated with chills and rigors.
Loss of appetite and loss of Weight are seen.
HISTORY OF PAST ILLNESS:
No H/O similar complaints in the past.
No H/O pulmonary tuberculosis and COVID -19.
No H/O diabetes, hypertension,CAD and epilepsy.
PERSONAL HISTORY:
Appetite: decreased
Diet: mixed
sleep: adequate
Bowel and bladder: Regular
addictions:H/o BD Smoking since 50 years (4-5 BD's per day)
FAMILY HISTORY:
Insignificant.
GENERAL EXAMINATION:
Patient is concious, coherent and oriented to time,place and person.
VITALS:
Pulse rate: 102 BPM
Respiratory rate: 26 CPM
BP: 110/80.
spO2: 96% at room air
SYSTEMIC EXAMINATION:
Respiratory system:
Inspection:
shape of the chest: Bilaterally symmetrical and elliptical.
chest movements: decreased on right side
no kyphosis and scoliosis
no scars( sinuse, visible pulsations and engorged veins)
no usage of accessory muscles.
muscle wasting- present
Palpation:
All inspectory findings are confirmed.
Trachea - shifted to right side.
No local rise of temperature.
chest movements- decreased on right side
spinoscapular distance- same on both sides.
chest expansion-
RT and Lt hemithorax
chest circumference- 31 cm
Transverse diameter- 27cm
anteroposterior diameter-20 cm
Percussion:
Right sided - ICA ( impaired note)
Right sided- SSA ( impaired note)
Auscultation:
Vesicular breath sounds are heard
RT sided - ISA and SSA ( decreased breath sounds)
RT - MA crepitus present.
Cardiac Examination:
S1 and S2 - present
Normal heart sounds
No cardiac murmurs.
CNS examination:
Superficial reflexes - present
sensory and motor functions- normal
no focal neurological deficits
Per Abdomen
bowel sounds- heard
soft, non tender,
no organomegaly
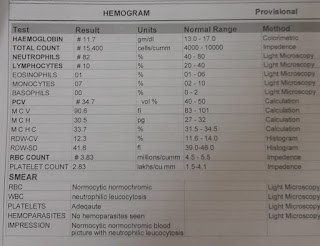
INVESTIGATIONS:
PROVISIONAL DIAGNOSIS:
Right Upper lobe fibrosis with pleural effusion.
TREATMENT:
Inj- AUGMENTIN ( 2g i.v TID)
Inj- PAN -40 mg OD
Inj- Paracetamol- 650 mg BD
ASCORIL - CS ( 2 table spoons)
Nebulization with Budecort ( BD )
Duolin ( TID)
O2 inhalation ( 2-4 lit/ min to maintain SpO2> 94%
Tab - Azithromycin ( 500 mg- OD)
A 45 year old female tailor by occupation came with
c/o headache with dragging sensation in the eyeballs since 3 days
Dropping of eyelid since 1 day
Double vision in the right eye since 1day
Vomitings since 3 days
HOPI: patient was apparently asymptomatic 1 month back.then she had diminision of vision for which she went to a ophthalmologist in nalgonda, they prescribed glasses for her eyesight. Then after using them for few days she got severe headache with dragging sensation in both the eyeballs. She went to a hospital in suryapet and was prescribed by pain killers.
Then next day she developed swelling of right eye, drooping of eyelid, double vision in right eye and vomitings since 3 days which was non bilious, non projectile
No h/o sudden onset weakness of limbs
No h/o any dizziness
Not a k/c/o DM, HTN, TB , ASTHMA, CVA, CAD
GENERAL EXAMINATION:
patient is c/c/c
No pallor, no icterus, cyanosis, clubbing,koilonychia lymphadenopathy.
VITALS:
Temperature: 98.6
Bp:130/90 mmhg
PR:56
RR: 20
Spo2: 99 on RA
Gcs:E4V5M6
CVS : S1 S2 heard
RS: BAE+
P/A: soft, non tender
CNS EXAMINATION:
Speech normal
Pupils normal
Cranial nerve -3
Left : normal
Right: lateral rectus+
Medial rectus -ve
Superior rectus -ve
Inferior rectus -ve
Sensory 6th intact
Other cranial nerves - intact
Tone : Rt Lt
UL Normal Normal
LL Normal Normal
Power: Rt Lt
UL 5/5 5/5
LL 5/5 5/5
Relfex:
Rt Lt
B - +2 +2
T - +2 +2
S- +2 +2
A - +2 +2
K - +2 +2
P- Flexor Flexor
neck stiffness -ve
Gait - normal
Investigations:
Diagnosis: pupil sparing 3rd nerve palsy
TREATMENT:
1. IVF - NS, RL @100ml/hr
2.INJ PAN 40mg IV/OD
3.INJ CIPLOX 200mg IV/BD
4.INJ METROGYL 100ml IV/TID
5.INJ ZOFER 4mg/IV/TID
6.INJ DICLOFENAC 75mg(3cc) IM/BD
7.VITALS MONITORING 4th hrly
8.INFORM SOS
13/5/22
S- no fresh complaints
O- right eye ptosis , mild conjuctival congestion
H/o lid swelling+, monocular diplopia, retropulsion+
Orbital movements:
rightt eye- abduction +
Left eye- all movements +
CN-3 no right lid elevation/medial rotation
Vitals:
Temp-afebrile
PR: 65
RR: 18
BP: 100/60
CVS-s1s2+
RS - BAE+
P/A- soft, non tender
A- 3rd CN palsy with pupillary sparing secondary to TOLOSA HUNT SYNDROME
P-
1. INJ METHYLPREDNISOLONE 1gm /IV OD IN 100ml NS
2.INJ PAN 40mg IV/OD
3VITALS MONITORING 4th hrly
4.INFORM SOS
14/5/22 day 3
S- no fresh complaints
O- right eye ptosis , chemosis resolved
lid swelling resolved, monocular diplopia, retropulsion+
Orbital movements:
rightt eye- abduction +
Elevation,depression,adduction,intorsion -absent
Left eye- all movements +
CN-3 no right lid elevation/medial rotation
Vitals:
Temp-afebrile
PR: 58
RR: 18
BP: 110/70
CVS-s1s2+
RS - BAE+
P/A- soft, non tender
A- 3rd CN palsy with pupillary sparing secondary to TOLOSA HUNT SYNDROME
P-
1. INJ METHYL PREDNISOLONE 1GM in 100 ml NS OD
2.INJ PAN 40mg IV/OD
3.VITALS MONITORING 4th hrly
4.INFORM SOS
15/5/22 day 4
S- no fresh complaints
O- right eye ptosis , chemosis resolved
lid swelling resolved
Ptosis +
Orbital movements:
rightt eye- abduction +
Elevation,depression,adduction,intorsion -absent
Left eye- all movements +
Vitals:
Temp-afebrile
PR: 64
RR: 18
BP: 160/80
CVS-s1s2+
RS - BAE+
P/A- soft, non tender
A- 3rd CN palsy with pupillary sparing secondary to TOLOSA HUNT SYNDROME
P-
1. INJ METHYL PREDNISOLONE 1GM in 100 ml NS OD
2.INJ PAN 40mg IV/OD
3.INJ HAI s/c acc to grbs
4.VITALS MONITORING 4th hrly
5.INFORM SOS
16/5/22 day 5
S- no fresh complaints
O- right eye ptosis , chemosis resolved
lid swelling resolved
Ptosis +
Orbital movements:
rightt eye- abduction +
Elevation,depression,adduction,intorsion -absent
Left eye- all movements +
Vitals:
Temp-afebrile
PR: 64
RR: 18
BP: 100/60
CVS-s1s2+
RS - BAE+
P/A- soft, non tender
A- 3rd CN palsy with pupillary sparing secondary to TOLOSA HUNT SYNDROME
P-
1. TAB METHYL PREDNISOLONE 1MG/KG PO/OD
2.TAB PAN 40mg PO/OD
3.INJ HAI s/c acc to grbs
4.VITALS MONITORING 4th hrly
















Comments
Post a Comment