1701006023 CASE PRESENTATION
LONG CASE
A 51 year old patient who is a resident of chitayala ,who works is a labourer in a goods company came to the hospital with chief complaints of:
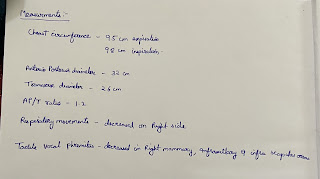
SYSTEMIC EXAMINATION :
Patient examined in sitting position
Inspection:-
oral cavity- Nicotine staining seen on teeth and gums ,nose,chest movements NORMAL
Respiratory movements appear to be decreased on right Side
Trachea is shifting towards left & Nipples are in 4th Intercoastal space
Apex impulse visible in 5th intercostal space.
NO SIGNS OF VOLUME LOSS
no dilated veins ,scars ,sinuses ,visible pulsations ,
no rib crowding ,no accessory muscle usage .
Palpation:-
All inspiratory findings are confirmed
Trachea is shifted
Apical impulse in left 5th ICS,
1cm medial to mid clavicular line
Respiratory movements decreased on right side
Tactile and vocal fremitus reduced on right side in infra axillary and infra scapular region
Gastrointestinal system :
Inspection -
-Abdomen DISTENDED
-All quadrants of abdomen are equally moving with respiration except Right upper quadrant
No visibe sinuses ,scars , visible pulsations or visible peristalsis
Palpation:
All inspectory findings are confirmed.
No tenderness .
Liver - is palpable 4 cm below the costal margin and moving with respiration.
Spleen : not palpable.
Kidneys - bimanually palpable.
Percussion - normal
Auscultation- bowel sounds heard .
No bruits .
Cardiovascular system -
S1 and S 2 heard in all areas ,no murmurs
Final Diagnosis :
Right sided Pleural effusion likely infectious etiology.
INVESTIGATIONS :
Pleural fluid analysis :
Colour - straw coloured
Total count -2250 cells
Differential count -60% Lymphocyte ,40% Neutrophils
No malignant cells.
Pleural fluid sugar = 128 mg/dl
Pleural fluid protein / serum protein= 5.1/7 = 0.7
Pleural fluid LDH / serum LDH = 0.6
Interpretation: Exudative pleural effusion.
Serology negative
Serum creatinine-0.8 mg/dl
CUE - normal
C/O fever on and off, associated with generalized body pains, loss of appetite for 3 months
C/O facial rash since 4-5 days
HISTORY OF PRESENT ILLNESS: Patient was apparently asymptomatic
10 years back then she developed joint pains, the fleeting type associated with morning stiffness for 10 min , not associated with swelling for 2 months for which she was treated at a private hospital and found to have?RA factor positive
patient was asymptomatic until 8 months back then she developed joint pains? post covid vaccination was treated at a private hospital with medications.
1 month back patient was having an episode of loss of consciousness with cold peripheries with sweating [grbs 7mg/dl] after taking Tab Glimi M2 prescribed by a local practitioner for high sugars?250mg/dl
10 days back patient developed fever and abdominal pain for which she was treated at a private hospital later she developed an erythematous rash over the face with itching, associated swelling of the left leg with erythema, and local rise of temperature[?cellulitis]
PAST HISTORY: Patient had a history of diminution of vision at age of 15 years started
using spectacles but there was gradual, progressive, painless loss of vision was certified as blind 2 years back .
No relevant drug, trauma history present
No similar complaints in family
Not a known case of DM/HTN/ASTHMA/CAD /EPILEPSY/TB
PERSONAL HISTORY:
Diet- mixed
Appetite- decreased
Bowel and bladder- regular
Sleep- disturbed
Addictions- nil
GENERAL EXAMINATION :
A 45-year-old female who is conscious coherent cooperative and well-oriented with time, place, and person
moderately built and nourished
Pallor +
no icterus, clubbing, cyanosis, lymphadenopathy, and edema
There is swelling in the left lower Limb on the lateral aspectWith itching, local rise pf of temperature and redness.Pigmentation is seen and swelling was associated with pain which is throbbing in nature non radiating type no aggrevating or releiving factors.
Dorsalis pedis artery is felt.
Erythematous rash is present on the cheek bilaterally.It is not associated with itching now. 10dsys back there was itching which was gradually subsided.
SYSTEMIC EXAMINATION;
CVS:
inspection shows no scars on the chest, no features of raised JVP, no additional visible pulsations seen
all inspectory findings are confirmed
apex beat normal at 5th ics medial to mcl
no additional palpable pulsations or murmurs
percussion showed normal heart borders
auscultation S1 S2 heard no murmurs or additional sounds
CNS: C/C/C
MOTOR-: normal tone and power
reflexes: RT LT
BICEPS ++ ++
TRICEPS ++ ++
SUPINATOR ++ ++
KNEE ++ ++
SENSORY :
touch, pressure, vibration, and proprioception are normal in all limbs
sensations could not be assessed at lt ll [dressing]
GIT:
inspection- normal scaphoid abdomen with no pulsations and scars
palpation - inspectory findings are confirmed
no organomegaly, non tender and soft
percussion- normal resonant note present, liver border normal
auscultation-normal abdominal sounds heard, no bruit present
RESPIRATORY:
inspection: normal chest shape bilaterally symmetrical, mediastinum central
no scars, Rr normal, no pulsations
palpation: Insp findings are confirmed
percussion: normal resonant note present bilaterally
INVESTIGATIONS:
Haematology : hemoglobin 6g/dl
X-rays :
Treatment:
1.INJ PIPTAZ 4.5 gm IV/ TID.
2.INJ METROGEL100 ML IV/TID
3.INJ NEOMOL1GM/IV/SOS
4.TAB CHYMORAL FORATE PO/TID
5.TAB PAN 40 MG PO/ OD.
6.TAB TECZINE10 MG PO/OD
7.TAB OROFERPO/OD.
8.TAB HIFENAC-P PO/OD
9HYDROCOTISONE cream 1%on face for 1week.
Provisional diagnosis :
SECONDARY SJOGRENS SYNDROME
LEFT LOWER LIMB CELLULITIS WITH BILATERAL OPTIC ATROPHY





























Comments
Post a Comment