Treatment:
INJ. MEROPENEM 500mg IV BD
INJ. ZOFER 4mg IV TID
INJ. PAN 40mg IV OD
IV Fluids- NS,RL @ 100 mL/hr
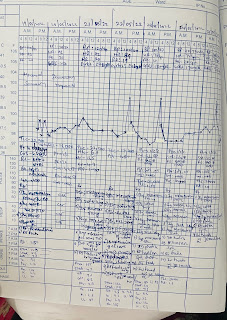
BP/HR/RR/SpO2 charting
Temp charting 4th hrly
RT feeds- 2nd hrly 100 mL water
SOAP NOTES:
DAY1
SOAP NOTES ICU BED-6, DAY -1
DOA: 19/05/2022
S:
C/o vomitting present
Pt is c/c/c
Pt is not drowsy
Pt c/o mild abdominal pain- diffuse
O:
BP: 120/70 mmHg
HR:96 bpm
RR: 20 cpm
TEMP: 98.7 F
SPO2:98% on RA
GRBS: 256 mg/dL
General Examination:
Pallor present
No Icterus/Cyanosis/Clubbing/Koilonychia/Lymphadenopathy/Edema
No dehydration
Thyroid normal
Systemic Examination:
CVS: S1S2 heard, No murmurs
RS: BAE+,NVBS
P/A: Soft, Non tender
CNS:
Pt is having altered sensorium
Reflexes: (Biceps/Triceps/Knee/Ankle/Plantar)-
+
Power: Normal(5/5) in both Upper and Lower limbs
Tone: Normal in both Upper and Lower limbs
No meningeal signs
A:
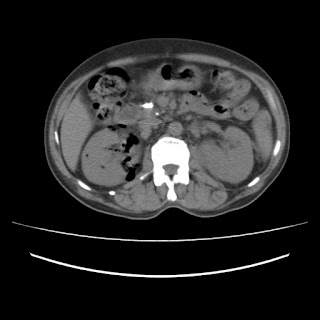
Right Emphysematous Pyelonephritis with Left Acute Pyelonephritis with Encephalopathy secondary to Sepsis
H/o Type 2 DM since 10 yrs
P:
INJ. MEROPENEM 500mg IV BD
INJ. ZOFER 4mg IV TID
INJ. PAN 40mg IV OD
IV Fluids- NS,RL @ 100 mL/hr
BP/HR/RR/SpO2 charting
Temp charting 4th hrly
RT feeds- 2nd hrly 100 mL water
DAY2
SOAP NOTES ICU BED-6, DAY -2
DOA: 19/05/2022
S:
C/o vomitting present
Pt is c/c/c
Pt is not drowsy
Pt c/o mild abdominal pain- diffuse
O:
BP: 120/70 mmHg
HR:96 bpm
RR: 20 cpm
TEMP: 98.7 F
SPO2:98% on RA
GRBS: 256 mg/dL
General Examination:
Pallor present
No Icterus/Cyanosis/Clubbing/Koilonychia/Lymphadenopathy/Edema
No dehydration
Thyroid normal
Systemic Examination:
CVS: S1S2 heard, No murmurs
RS: BAE+,NVBS
P/A: Soft, Non tender
CNS:
Pt is having altered sensorium
Reflexes: (Biceps/Triceps/Knee/Ankle/Plantar)-
+
Power: Normal(5/5) in both Upper and Lower limbs
Tone: Normal in both Upper and Lower limbs
No meningeal signs
A:
Right Emphysematous Pyelonephritis with Left Acute Pyelonephritis with Encephalopathy secondary to Sepsis
H/o Type 2 DM since 10 yrs
P:
INJ. MEROPENEM 500mg IV BD
INJ. ZOFER 4mg IV TID
INJ. PAN 40mg IV OD
IV Fluids- NS,RL @ 100 mL/hr
BP/HR/RR/SpO2 charting
Temp charting 4th hrly
RT feeds- 2nd hrly 100 mL water
DAY4
SOAP NOTES ICU BED-6, DAY -4
DOA: 19/05/2022
S:
No new complaints
O:
BP: 100/60 mmHg
HR:76 bpm
RR: 20 cpm
TEMP: 98.7 F
SPO2:98% on RA
GRBS: 148 mg/dL
General Examination:
Pallor present
No Icterus/Cyanosis/Clubbing/Koilonychia/Lymphadenopathy/Edema
No dehydration
Thyroid normal
Systemic Examination:
CVS: S1S2 heard, No murmurs
RS: BAE+,NVBS
P/A: Soft, Non tender
CNS:
NAD
Reflexes: (Biceps/Triceps/Knee/Ankle/Plantar)-
+
Power: Normal(5/5) in both Upper and Lower limbs
Tone: Normal in both Upper and Lower limbs
No meningeal signs
A:
Right Emphysematous Pyelonephritis with Left Acute Pyelonephritis with Encephalopathy secondary to Sepsis
H/o Type 2 DM since 10 yrs
P:
INJ. MEROPENEM 500mg IV BD
INJ. ZOFER 4mg IV TID
INJ. RANTAC 50mg IV OD
INJ. KCl 2 Amp in 500 mL NS over 4.5 hrs infusion
IV Fluids- NS,RL @ 100 mL/hr
SYP. POTCHLOR 10 mL in 1 glass of water TID
SYP. MUCAINE GEL 10 mL PO TID
7 point profile
BP/HR/RR/SpO2 charting
Temp charting 4th hrly
RT feeds- 2nd hrly 100 mL water
DAY5
SOAP NOTES ICU BED-6, DAY -5
DOA: 19/05/2022
S:
No new complaints
O:
BP: 100/60 mmHg
HR:78 bpm
RR: 20 cpm
TEMP: 98.7 F
SPO2:98% on RA
GRBS: 148 mg/dL
I/O:2950mL/1700mL
General Examination:
Pallor present
No Icterus/Cyanosis/Clubbing/Koilonychia/Lymphadenopathy/Edema
No dehydration
Thyroid normal
Systemic Examination:
CVS: S1S2 heard, No murmurs
RS: BAE+,NVBS
P/A: Soft, Non tender
CNS:
NAD
Reflexes: (Biceps/Triceps/Knee/Ankle/Plantar)-
+
Power: Normal(5/5) in both Upper and Lower limbs
Tone: Normal in both Upper and Lower limbs
No meningeal signs
A:
Right Emphysematous Pyelonephritis with Left Acute Pyelonephritis with Encephalopathy secondary to Sepsis
H/o Type 2 DM since 10 yrs
P:
INJ. MEROPENEM 500mg IV BD
INJ. ZOFER 4mg IV TID
INJ. RANTAC 50mg IV OD
INJ. KCl 2 Amp in 500 mL NS over 4.5 hrs infusion
IV Fluids- NS,RL @ 100 mL/hr
SYP. POTCHLOR 10 mL in 1 glass of water TID
SYP. MUCAINE GEL 10 mL PO TID
7 point profile
BP/HR/RR/SpO2 charting
Temp charting 4th hrly
RT feeds- 2nd hrly 100 mL water
DAY6
SOAP NOTES ICU BED-6, DAY -6
DOA: 19/05/2022
S:
Diffuse abdominal pain present aggravated upon consuming food
1 fever spike yesterday evening
Encephalopathy resolving
No other complaints
O:
BP: 110/70 mmHg
HR:74 bpm
RR: 20 cpm
TEMP: 98.3 F
SPO2:98% on RA
GRBS: 170 mg/dL
General Examination:
Pallor present
No Icterus/Cyanosis/Clubbing/Koilonychia/Lymphadenopathy/Edema
No dehydration
Thyroid normal
Systemic Examination:
CVS: S1S2 heard, No murmurs
RS: BAE+,NVBS
P/A: Soft, Non tender
CNS:
NAD
Reflexes: (Biceps/Triceps/Knee/Ankle/Plantar)-
+
Power: Normal(5/5) in both Upper and Lower limbs
Tone: Normal in both Upper and Lower limbs
No meningeal signs
A:
Right Emphysematous Pyelonephritis with Left Acute Pyelonephritis with Encephalopathy secondary to Sepsis
H/o Type 2 DM since 10 yrs
P:
INJ. MEROPENEM 500mg IV BD (Day 6)
INJ. ZOFER 4mg IV TID
INJ. RANTAC 50mg IV OD
INJ. LASIX 40 mg IV BD
IV Fluids- NS,RL @ 100 mL/hr
SYP. MUCAINE GEL 10 mL PO TID
GRBS 7 point profile
INJ.HAI SC TID ACC to GRBS
TAB.DOLO 650 mg SOS
BP/HR/RR/SpO2 charting
Temp charting 4th hrly
DAY7
SOAP NOTES ICU BED-6, DAY -7
DOA: 19/05/2022
S:
No complaints
O:
BP: 110/70 mmHg
HR:72 bpm
RR: 20 cpm
TEMP: 98.3 F
SPO2:98% on RA
GRBS: 215 mg/dL
General Examination:
Pallor present
No Icterus/Cyanosis/Clubbing/Koilonychia/Lymphadenopathy/Edema
No dehydration
Thyroid normal
Systemic Examination:
CVS: S1S2 heard, No murmurs
RS: BAE+,NVBS
P/A: Soft, Non tender
CNS:
NAD
Reflexes: (Biceps/Triceps/Knee/Ankle/Plantar)-
+
Power: Normal(5/5) in both Upper and Lower limbs
Tone: Normal in both Upper and Lower limbs
No meningeal signs
A:
Right Emphysematous Pyelonephritis with Left Acute Pyelonephritis with Encephalopathy secondary to Sepsis
H/o Type 2 DM since 10 yrs
P:
INJ. MEROPENEM 500mg IV BD (Day 7)
INJ. ZOFER 4mg IV TID
INJ. RANTAC 50mg IV OD
INJ. LASIX 40 mg IV BD
IV Fluids- NS,RL @ 100 mL/hr
SYP. MUCAINE GEL 10 mL PO TID
GRBS 7 point profile
INJ.HAI SC TID ACC to GRBS
TAB.DOLO 650 mg SOS
BP/HR/RR/SpO2 charting
Temp charting 4th hrly
DAY8
SOAP NOTES ICU BED-6, DAY -8
DOA: 19/05/2022
S:
1 fever spike since yesterday
Sensorium improving
Abdominal pain subsided
O:
BP: 110/70 mmHg
HR:74 bpm
RR: 20 cpm
TEMP: 98.3 F
SPO2:98% on RA
GRBS: 215 mg/dL
General Examination:
Pallor present
No Icterus/Cyanosis/Clubbing/Koilonychia/Lymphadenopathy/Edema
No dehydration
Thyroid normal
Systemic Examination:
CVS: S1S2 heard, No murmurs
RS: BAE+,NVBS
P/A: Soft, Non tender
CNS:
NAD
Reflexes: (Biceps/Triceps/Knee/Ankle/Plantar)-
+
Power: Normal(5/5) in both Upper and Lower limbs
Tone: Normal in both Upper and Lower limbs
No meningeal signs
A:
Right Emphysematous Pyelonephritis with Left Acute Pyelonephritis with Encephalopathy secondary to Sepsis
H/o Type 2 DM since 10 yrs
P:
NBM till further orders
INJ. MEROPENEM 500mg IV BD (Day 8)
INJ. ZOFER 4mg IV TID
INJ. RANTAC 50mg IV OD
INJ. LASIX 40 mg IV BD
IV Fluids- NS,RL @ 100 mL/hr
SYP. MUCAINE GEL 10 mL PO TID
GRBS 7 point profile
INJ.HAI SC TID ACC to GRBS
TAB.DOLO 650 mg SOS
BP/HR/RR/SpO2 charting
Temp charting 4th hrly
DAY9
SOAP NOTES ICU BED-6, DAY -9
DOA: 19/05/2022
S:
Sensorium improving
Abdominal pain subsided
O:
BP: 120/70 mmHg
HR:72 bpm
RR: 20 cpm
TEMP: 98.3 F
SPO2:98% on RA
GRBS: 164 mg/dL
General Examination:
Pallor present
No Icterus/Cyanosis/Clubbing/Koilonychia/Lymphadenopathy/Edema
No dehydration
Thyroid normal
Systemic Examination:
CVS: S1S2 heard, No murmurs
RS: BAE+,NVBS
P/A: Soft, Non tender
CNS:
NAD
Reflexes: (Biceps/Triceps/Knee/Ankle/Plantar)-
+
Power: Normal(5/5) in both Upper and Lower limbs
Tone: Normal in both Upper and Lower limbs
No meningeal signs
A:
Right Emphysematous Pyelonephritis with Left Acute Pyelonephritis with Encephalopathy secondary to Sepsis
H/o Type 2 DM since 10 yrs
P:
NBM till further orders
INJ. MEROPENEM 500mg IV BD (Day 9)
INJ. ZOFER 4mg IV TID
INJ. RANTAC 50mg IV OD
INJ. LASIX 40 mg IV BD
IV Fluids- NS,RL @ 100 mL/hr
SYP. MUCAINE GEL 10 mL PO TID
GRBS 7 point profile
INJ.HAI SC TID ACC to GRBS
TAB.DOLO 650 mg SOS
BP/HR/RR/SpO2 charting
Temp charting 4th hrly
SDP Transfusion done I/v/o low platelet count
Pre transfusion counts
Hb: 7.0 g/dL
TLC:22000
PLt:26000
Post transfusion counts
Hb:6.5 g/dL
TLC: 17700
PLt:7000
DAY 10
SOAP NOTES ICU BED-6, DAY -9
DOA: 19/05/2022
S:
Sensorium improving
Abdominal pain subsided
O:
BP: 120/70 mmHg
HR:72 bpm
RR: 20 cpm
TEMP: 98.3 F
SPO2:98% on RA
GRBS: 164 mg/dL
General Examination:
Pallor present
No Icterus/Cyanosis/Clubbing/Koilonychia/Lymphadenopathy/Edema
No dehydration
Thyroid normal
Systemic Examination:
CVS: S1S2 heard, No murmurs
RS: BAE+,NVBS
P/A: Soft, Non tender
CNS:
NAD
Reflexes: (Biceps/Triceps/Knee/Ankle/Plantar)-
+
Power: Normal(5/5) in both Upper and Lower limbs
Tone: Normal in both Upper and Lower limbs
No meningeal signs
A:
Right Emphysematous Pyelonephritis with Left Acute Pyelonephritis with Encephalopathy secondary to Sepsis
H/o Type 2 DM since 10 yrs
P:
NBM till further orders
INJ. MEROPENEM 500mg IV BD (Day 10)
INJ. COLISTIN IV OD
INJ. ZOFER 4mg IV TID
INJ. RANTAC 50mg IV OD
INJ. LASIX 40 mg IV BD
IV Fluids- NS,RL @ 100 mL/hr
SYP. MUCAINE GEL 10 mL PO TID
GRBS 7 point profile
INJ.HAI SC TID ACC to GRBS
TAB.DOLO 650 mg SOS
BP/HR/RR/SpO2 charting
Temp charting 4th hrly
DAY 12
SOAP NOTES ICU BED-6, DAY -12
DOA: 19/05/2022
S:
Previous complaints resolving
O:
BP: 110/80 mmHg
HR:89 bpm
RR: 20 cpm
TEMP: 99.7 F
SPO2:98% on RA
GRBS: 148 mg/dL
General Examination:
Pallor present
No Icterus/Cyanosis/Clubbing/Koilonychia/Lymphadenopathy/Edema
No dehydration
Thyroid normal
Systemic Examination:
CVS: S1S2 heard, No murmurs
RS: BAE+,NVBS
P/A: Soft, Non tender
CNS:
NAD
Reflexes: (Biceps/Triceps/Knee/Ankle/Plantar)-
+
Power: Normal(5/5) in both Upper and Lower limbs
Tone: Normal in both Upper and Lower limbs
No meningeal signs
A:
Right Emphysematous Pyelonephritis with Left Acute Pyelonephritis with Encephalopathy secondary to Sepsis
H/o Type 2 DM since 10 yrs
P:
INJ. COLISTIN 2.25 MU IV OD(Day 5)
INJ. ZOFER 4mg IV TID
INJ. RANTAC 50mg IV OD
INJ. LASIX 40 mg IV BD
IV Fluids- NS,RL @ 100 mL/hr
SYP. MUCAINE GEL 10 mL PO TID
GRBS 7 point profile
INJ.HAI SC TID ACC to GRBS
TAB.DOLO 650 mg SOS
BP/HR/RR/SpO2 charting
Temp charting hrly
-------------------------------------------------------------------------------------------------------------------------------------
SHORT CASE
This is a case of 50 years old patient, who is a farmer by occupation, resident of pochampally has presented to the casualty 7 days back with the chief complaints of
- Abdominal distension since 8 days
- Pain in the abdomen since 8 days
- Pedal edema since 6 days
5Am-Wake up
Till 8AM- Field work
8AM- Breakfast (Rice)
1PM - lunch
6PM- reaches home
8PM - dinner
9PM - sleep
The Patient was apparently asymptomatic 6 months ago when he developed jaundice and was treated in a private hospital
His last consumption of alcohol was on 29th May 2022 which was when he drank more than usual
Then he developed abdominal distension which was insidious in onset and gradually progressive to the present size
There were no aggravating and relieving factors
It was associated with
1)pain abdomen in the epigastric and right hypochondriac region which is insidious in onset and diffuse to whole of the abdomen and gradually increased in intensity and is of colicky type
Pain is persistent throughout the day. No history of radiation to the back.
2) bilateral pedal edema below knees and is of pitting type, which was insidious in onset and gradually progressive throughout the day and is maximum in the evening and is not relieved by rest
No local rise of temperature and tenderness
Associated symptoms- shortness of breath since 4 days
There is no history of orthopnoea, PND or palpitations
No history of facial puffiness and haematuria
No history of evening rise of temperature, cough, night sweats
No history suggestive of hemetemesis, melena, bleeding per rectum
No raised JVP, basal lung crepitations
No palpable mass per abdomen
Past history
No history of similar complaints in the past
Not a known case of Hypertension, Diabetes, asthma, epilepsy, TB
No previous surgical history
Personal history
Diet- Mixed
Appetite- Decreased since 10 days
Bowel and bladder movements- Regular
Sleep- Adequate
Addictions-
Patient is a chronic smoker since 30 years- 4to5 beedis/day
Alcohol - Consuming whisky since 20 years- 3 to 4 times per week (90 ml each time)
No history of drug or food allergies
Family history
No similar complaints in the family
General examination
Done after obtaining consent, in the presence of attendant with adequate exposure
Patient is conscious, coherent, cooperative and well oriented to time, place and person
Patient is well nourished and moderately built
Pallor - absent
Icterus- present
Cyanosis- absent
Clubbing- absent
Pedal edema- present- bilateral pitting type
Lymphadenopathy- absent
Vitals
Temperature- Afebrile
Blood pressure- 120/80 mm of Hg
Pulse rate- 78 bpm
Respiratory rate- 16 cpm
Local examination
Abdominal examination:
Inspection
Shape of the abdomen- Distended
Umbilicus- everted
Movements of abdominal wall- moves with respiration
Skin is smooth, shiny
No visible peristalsis, pulsations, sinuses, engorged veins, hernial sites
Palpation
Inspectory findings are confirmed
Tenderness is present in whole of the abdomen
Guarding and rigidity present
Fluid thrill positive
No hepatosplenomegaly
Percussion
Fluid thrill- felt
Liver span- Not detectable
Auscultation
Bowel sounds are heard
Cardiovascular system examination:
S1 and S2 sounds are heard
No murmurs
Respiratory system examination:
Bilateral air entry present
Normal vesicular breath sounds are heard
Central nervous system examination:
No focal neurological deficits
Investigations
Investigations:
Serology
HIV- Negative
HCV- Negative
HbsAg- Negative
HemogramHaemoglobin- 9.8 gm/dl
Total count- 7200 cells/cumm
Neutrophils- 49%
Lymphocyes- 40%
Eosinophils- 1%
Monocytes- 10%
PCV- 27.4 vol%
MCH- 33 pg
MCHC- 35.8%
RDW- 17.6
RBC count- 2.97 millions/cumm
Prothrombin time
Prothrombin time- 16 sec
INR- 1.11
Ascitic fluid protein sugar
Sugar- 95 mg/dl
Protein- 0.6 g/dl
Ascitic fluid for LDH
LDH- 29.3 IU/L
Blood Urea
Blood urea- 12mg/dl
ESR
ESR- 15mm/1st hour
LFT
Total bilirubin- 2.22 mg/dl
Direct bilirubin- 1.13 mg/dl
SGOT(AST)- 147 IU/L
SGPT(ALT)- 48 IU/L
Alkaline phosphate- 204 IU/L
Total proteins- 6.3 gm/dl
Albumin- 3 gm/dl
Serum electrolytes
Sodium- 133 mEq/L
Potassium- 3 mEq/L
Chloride- 94 mEq/L
Serum creatinine
Serum creatinine- 0.8 mg/dl
APTT
APTT test- 32 sec
SAAG
Serum albumin- 3 gm/dl
Ascitic albumin- 0.34 gm/dl
SAAG- 2.66
Provisional diagnosis:
Acute decompensated liver failure with ascites
Treatment:
1. Inj PAN 40 mg IV/OD
2. Inj LASIX 40mg IV/BD
3. Tab Spiranolactone 50mg/ BD
4. Inj Thiamine 1 amp in 100 ml NS IV/ TID
5. Syrup lactulose 15 ml/ TID
6. Abdominal girth charting 4th hourly
7. Fluid restriction <1L/ day
8. Salt restriction <2g/ day
Ascitic fluid tapping
Ascitic fluid was tapped twice- on 2nd June 2022 & 6th June 2022













































Comments
Post a Comment