1701006034 CASE PRESENTATION
LONG CASE
CHIEF COMPLAINTS-
A 70 yr old man presented to the OPD on 06/06/22 with chief complaints of:
- Weakness of right upper and lower limb since 3 days.
- Slurring of speech since 3 days
- Drooling of saliva since 3 days.
HISTORY OF PRESENTING ILLNESS-
Patient was apparently asymptomatic 3 years ago when he developed sudden onset weakness of right upper and lower limbs, without slurring of speech. After being treated, he then recovered from it. After 2 years (a year ago) he developed a second episode of sudden onset weakness of right upper and lower limbs, that was associated with drooping of mouth, drooling of saliva, slurring of speech. He was again treated for it and recovered completely. He then had a third episode of sudden onset weakness of right upper and lower limbs 4 days ago. He also had drooping of mouth on one side, drooling of saliva, slurring of speech associated with right sided weakness of the limbs.
No history of involuntary movements, urinary incontinence.
No history of nausea and vomiting.
No h/o head injury, up rolling of eye balls.
PAST HISTORY-
Patient is a k/c/o hypertension since 1 year and is on regular medications (Tab. Atenolol 25mg).
Patient is not a k/c/o diabetes mellitus, TB, epilepsy, asthma.
FAMILY HISTORY-
No history of similar complaints in the family.
No history of DM, TB, Stroke, Asthma, or any other hereditary diseases in the family.
TREATMENT HISTORY-
On medication for hypertension (Tab. Atenolol 25mg).
PERSONAL HISTORY-
Appetite: Normal
Diet: Mixed
Bowel movements: Regular
Bladder movements: Normal
Sleep: Adequate
No known allergies
History of alcohol addiction that stopped 5 years ago.
No other addictions.
GENERAL EXAMINATION-
The patient is examined in a well lit room with informed consent.
The patient is conscious, coherent and cooperative and is well oriented to time, place and person.
He is moderately built and well nourished.
Pallor: Absent
Icterus: Absent
Cyanosis: Absent
Clubbing: Absent
Lymphadenopathy: Absent
Edema: Absent
VITALS-
On 06/06/22 (At the time of admission):
Temperature- Afebrile
Heart Rate- 70 BPM
Blood Pressure- 140/80 mm of Hg
Respiratory rate- 16/min
SPO2- 98% at room air
On 07/06/22:
Temperature- Afebrile
Heart Rate- 80 BPM
Blood Pressure- 130/80 mm of Hg
FBS- 158mg/dl
GRBS- 167mg/dl
SYSTEMIC EXAMINATION-
CVS SYSTEM: S1,S2 heard
No added thrills, no murmurs
RESPIRATORY SYSTEM:
Dyspnea: Absent
Wheeze: Absent
Position of trachea: Central
Breath sounds: Vesicular breath sounds heard
Adventitious sounds: Not heard
PER ABDOMEN:
Soft, non tender, no organomegaly
CNS:
Patient is conscious/alert.
Speech-slurred
No signs of meningeal irritation
Cranial nerves- NAD
Sensory system- NAD
Motor system-
Right Left
Tone- UL Decreased Normal
LL Decreased Normal
Power- UL 0/5 4/5
LL 0/5 4/5
REFLEXES-
Biceps- +++ ++
Triceps- +++ ++
Supinator- +++ ++
Knee- +++ ++
Ankle- +++ ++
INVESTIGATIONS-
Blood group- A+ve
Hemogram-
Hb%- 12.6gm/dl
TLC- 8,600 cells/cumm3
RBC- 4.33million cells
Neutrophils- 55%
lymphocytes- 35%
Eosinophils- 03%
Blood Urea- 24mg/dl
Serum creatinine- 1.3mg/dl
Serum electrolytes-
Sodium- 136mEq/L
Potassium- 3.7mEq/L
Chloride- 104mEq/L
LFT-
Total bilirubin- 0.61mg/dl
Direct bilirubin- 0.16mg/dl
SGPT- 11 units/L
SGOT- 13 units/L
Alkaline phosphate- 105 IU/L
Albumin- 4g/dl
A/G Ratio- 1.71
PT- 2min
ECG-
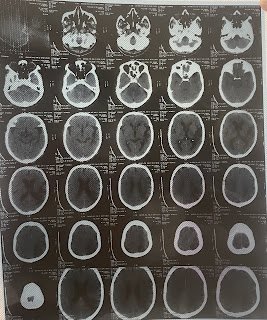
MRI-
Present-
1yr ago-
PROVISIONAL DIAGNOSIS-
Acute ischemic stroke causing right sided hemiplegia (left MCA territory)
Recurrent CVA
TREATMENT-
Tab Ecospirin 150mg PO OD
Tab Clopidogrel 75mg PO OD
Tab Atorvas 40mg PO HS
Tab Pan 40mg PO OD
Tab Aten 25mg PO OD
Physiotherapy of right upper and lower limbs
Monitoring vitals
------------------------------------------------------------------------------------------------------------------------------------
SHORT CASE
CHIEF COMPLAINTS-
A 71 yr old man presented to the OPD with chief complaints of:
- Shortness of breath since 25 days.
- Cough with sputum since 25 days
- Fever since 9 days.
HISTORY OF PRESENTING ILLNESS-
-Patient was apparently asymptomatic 25 days ago when he developed Grade 2-3 shortness of breath, that was aggravated on exertion, exposure to cold air, relieved by rest. It was insidious in onset. It was associated with wheeze. No history of orthopnea or PND.
-Cough with expectoration was non foul smelling, non blood stained. Sputum was mucoid. It increased during nights. No postural or diurnal variations. It was relieved on taking medications.
-Fever was low grade, continuous. No evening rise of temperature, not associated with chills. It was relieved on medication.
-There was loss of appetite and weight.
PAST HISTORY-
No history of pulmonary TB or covid 19 in the past.
No similar complaints in the past.
Not a k/c/o Diabetes mellitus, Hypertension, CAD, Epilepsy.
FAMILY HISTORY-
No history of similar complaints in the family.
No history of DM, TB, Stroke, Asthma, or any other hereditary diseases in the family.
TREATMENT HISTORY-
Not on any medications.
PERSONAL HISTORY-
Appetite: reduced
Diet: Mixed
Bowel movements: Regular
Bladder movements: Normal
Sleep: Adequate
No known allergies
History of smoking- 50 pack years.
No other addictions.
GENERAL EXAMINATION-
The patient is examined in a well lit room with informed consent.
The patient is conscious, coherent and cooperative and is well oriented to time, place and person.
He is thin built and malnourished.
Weight- 34kg
Pallor: Present
Icterus: Absent
Cyanosis: Absent
Clubbing: Absent
Lymphadenopathy: Absent
Edema: Absent
VITALS-
On 02/06/22:
Heart Rate- 102 BPM
Blood Pressure- 120/80 mm of Hg
Respiratory rate- 26/min
SPO2- 90% at room air
On 03/06/22:
Heart Rate- 89 BPM
Blood Pressure- 120/80 mm of Hg
Respiratory rate- 26/min
SPO2- 96% at room air
On 04/06/22:
Heart Rate- 94 BPM
Blood Pressure- 120/80 mm of Hg
Respiratory rate- 24/min
SPO2- 92% at room air
Temperature-98.4F
On 05/06/22:
Heart Rate- 90 BPM
Blood Pressure- 120/80 mm of Hg
Respiratory rate- 24/min
SPO2- 96% at room air
On 06/06/22:
Heart Rate- 88 BPM
Blood Pressure- 120/80 mm of Hg
Respiratory rate- 22/min
SPO2- 98% at room air
On 07/06/22:
Heart Rate- 92 BPM
Blood Pressure- 120/80 mm of Hg
Respiratory rate- 24/min
SPO2- 91% at room air
SYSTEMIC EXAMINATION-
CVS SYSTEM: S1,S2 heard
No added thrills, no murmurs
RESPIRATORY SYSTEM:
Dyspnea: Present
Wheeze: Present
Position of trachea: Shifted to right
Inspection-
Shape of chest-B/L symmetrical, elliptical.
Chest movements decreased on right side.
No kyphosis, or scoliosis.
No crowding of ribs.
No scars, sinuses, visible pulsations or engorged veins.
No wasting of muscles
No usage of accessory muscles.
Palpation-
All inspectory findings are confirmed.
Trachea shifted to right side.
No local rise of temp.
Chest movements decreased on right side.
Percussion-
Right side ICA impaired note
Right SSA impaired
TVF equal on BS.
Auscultation-
Vesicular breath sounds
Right SSA + LSA decreased breath sounds
Right MA crepts +ve.
PER ABDOMEN:
Soft, non tender, no organomegaly
CNS: Intact
INVESTIGATIONS-
TREATMENT-
On 1/6/22-
Tab. AUGMENTIN 1.2gm IV TID
Tab. PAN 40mg OD
Tab. PCM 650mg BD
Syrup ASCORIL-LS 2Tbsp
Neb. with BUDECORT BD
DOULIN TID
MUCOMAL TID
O2 inhalation with nasal prongs @ 2-4L/min
Maintain spO2 > 94%
Tab. AZEE 500mg OD
On 2/6/22-
Tab. AUGMENTIN 1.2gm IV TID
Tab. PAN 40mg OD
Tab. PCM 650mg BD
Syrup ASCORIL-LS 2Tbsp
Neb. with BUDECORT BD
DOULIN TID
MUCOMAL TID
O2 inhalation with nasal prongs @ 2-4L/min
Maintain spO2 > 94%
Tab. AZEE 500mg OD
On 3/6/22-
Tab. AUGMENTIN 1.2gm IV TID
Tab. PAN 40mg OD
Tab. PCM 650mg BD
Syrup ASCORIL-LS 2Tbsp
Neb. with BUDECORT BD
DOULIN TID
MUCOMAL TID
O2 inhalation with nasal prongs @ 2-4L/min
Maintain spO2 > 94%
Tab. AZEE 500mg OD
Syrup CREMAFFIN 10ml HS
On 4/6/22-
Tab. AUGMENTIN 1.2gm IV TID
Tab. PAN 40mg OD
Tab. PCM 650mg BD
Syrup ASCORIL-LS 2Tbsp
Neb. with BUDECORT BD
DOULIN TID
MUCOMAL TID
O2 inhalation with nasal prongs @ 2-4L/min
Maintain spO2 > 94%
Tab. AZEE 500mg OD
Syrup CREMAFFIN 10ml HS
Inj. OPYINEURON IV
Tab. ACECLO-TH BD
On 5/6/22-
Tab. AUGMENTIN 1.2gm IV TID
Tab. PAN 40mg OD
Tab. PCM 650mg BD
Syrup ASCORIL-LS 2Tbsp
Neb. with BUDECORT BD
DOULIN TID
MUCOMAL TID
O2 inhalation with nasal prongs @ 2-4L/min
Maintain spO2 > 94%
Tab. AZEE 500mg OD
Syrup CREMAFFIN 10ml HS
Inj. OPYINEURON IV
Tab. ACECLO-TH BD
Needle thoracocentesis-
Done under aseptic conditions. Done under the guidance of USG. Betadine was painted at 5th ICS on right side, mid clavicular line. 2% Xylocaine was instilled and a 20CC syringe was inserted and pleural fluid was aspirated of about 20ml which was straw colored. Procedure was uneventful.
Post procedure vitals-
PR- 100BPM
BP- 120/80mmhg
RR- 24CPM
spO2- 94% @ RA
On 6/6/22-
Tab. AUGMENTIN 1.2gm IV TID
Tab. PAN 40mg OD
Tab. PCM 650mg BD
Syrup ASCORIL-LS 2Tbsp
Neb. with BUDECORT BD
DOULIN TID
MUCOMAL TID
O2 inhalation with nasal prongs @ 2-4L/min
Maintain spO2 > 94%
Tab. AZEE 500mg OD
Syrup CREMAFFIN 10ml HS
Inj. OPYINEURON IV
Tab. ACECLO-TH BD
On 7/6/22-
Tab. AUGMENTIN 1.2gm IV TID
Tab. PAN 40mg OD
Tab. PCM 650mg BD
Syrup ASCORIL-LS 2Tbsp
Neb. with BUDECORT BD
DOULIN TID
MUCOMAL TID
O2 inhalation with nasal prongs @ 2-4L/min
Maintain spO2 > 94%
Tab. AZEE 500mg OD
Syrup CREMAFFIN 10ml HS
Tab. ACECLO-TH BD
Diclofenac patch











Comments
Post a Comment