1701006046 CASE PRESENTATION
LONG CASE
A 50 years old male who is a farmer by occupation, resident of pochampally has presented to the casualty on 02 June 2022 with the chief complaints of
- Abdominal distension since 8 days
- Pain in the abdomen since 8 days
- Pedal edema since 6 days
History of presenting illness:
Patient was apparently asymptomatic 6 months ago when he developed jaundice and was treated in a private hospital
Then he developed abdominal distension 8 days ago which was insidious in onset and gradually progressive to the present size
There were no aggravating and relieving factors
His last consumption of alcohol was on 29th May 2022
It was associated with pain abdomen in the epigastric and right hypochondriac region which is insidious in onset and diffuse to whole of the abdomen and gradually increased in intensity and is of colicky type
Pain is persistent throughout the day. No history of radiation to the back.
No complaints of fever, nausea and vomiting
There were no aggravating and relieving factors
It was associated with bilateral pedal edema below knees and is of pitting type, which was insidious in onset and gradually progressive throughout the day and is maximum in the evening and is not relieved by rest
No local rise of temperature and tenderness
Associated symptoms- shortness of breath since 4 days
There is no history of orthopnoea, PND or palpitationsNo history of facial puffiness and haematuriaNo history of evening rise of temperature, cough, night sweatsNo history suggestive of hemetemesis, melena, bleeding per rectum No raised JVP, basal lung crepitationsNo palpable mass per abdomen
Daily routinePatient usually wakes up at 5 am and goes to field and comes home at 8 am and has rice for breakfast and returns to work at 9 amAt 1 pm he will have his lunchThen he goes to work from 2 pm to 6 pm and at 6 pm he comes to home At 8 pm he will have his dinner and at 9:30 pm he goes to sleep
Past historyNo history of similar complaints in the pastNot a known case of Hypertension, Diabetes, asthma, epilepsy, TBNo previous surgical history
Personal historyDiet- MixedAppetite- Decreased since 10 daysBowel and bladder movements- Urine frequency is reduced since 3 days and patient has an history of constipationSleep- AdequateAddictions-Patient is a chronic smoker since 30 years- 4to5 beedis/dayAlcohol - Consuming whisky since 20 years- 3 to 4 times per week (90 ml each time), but stopped consuming regularly 6 months backPatient consumes toddy occasionallyNo history of drug or food allergies
Family historyNo similar complaints in the family
General examinationDone after obtaining consent, in the presence of attendant with adequate exposurePatient is conscious, coherent, cooperative and well oriented to time, place and personPatient is well nourished and moderately built Icterus is positivePedal edema- present- bilateral pitting type
No history of pallor, cyanosis, clubbing and lymphadenopathy
VitalsTemperature- AfebrileBlood pressure- 120/80 mm of HgPulse rate- 78 bpmRespiratory rate- 16 cpm
EXAMINATION OF HANDS AND ARMS :Tremors were present.
Local examinationAbdominal examination:
InspectionShape of the abdomen- DistendedUmbilicus- evertedMovements of abdominal wall- moves with respirationSkin is smooth, shinyNo visible peristalsis, pulsations, sinuses, engorged veins, hernial sitesPalpationInspectory findings are confirmedTenderness is present in whole of the abdomenGuarding and rigidity presentFluid thrill positiveNo hepatosplenomegalyAbdominal girth at the level of umbilicus is maximum
PercussionTympanic note is heard on the midline and dull note is heard on the flanks in supine positionFluid thrill- felt Liver span- Not detectable
AuscultationBowel sounds are decreased
Cardiovascular system examination:S1 and S2 sounds are heardNo murmurs
Respiratory system examination:Bilateral air entry presentNormal vesicular breath sounds are heard
Central nervous system examination:No focal neurological deficits
Investigations:
SerologyHIV- NegativeHCV- NegativeHbsAg- Negative
Hemogram
EXAMINATION OF HANDS AND ARMS :
Tremors were present.
Haemoglobin- 9.8 gm/dl
ECG
Colour doppler
Ascitic fluid cytology report
Bacterial culture & sensitivity report
Ascitic fluid protein sugarSugar- 95 mg/dlProtein- 0.6 g/dl
Ascitic fluid for LDHLDH- 29.3 IU/L
Blood UreaBlood urea- 12mg/dl
ESRESR- 15mm/1st hour
LFTTotal bilirubin- 2.22 mg/dlDirect bilirubin- 1.13 mg/dlSGOT(AST)- 147 IU/LSGPT(ALT)- 48 IU/LAlkaline phosphate- 204 IU/LTotal proteins- 6.3 gm/dlAlbumin- 3 gm/dl
Total count- 7200 cells/cummNeutrophils- 49%Lymphocyes- 40%Eosinophils- 1%Monocytes- 10%PCV- 27.4 vol%MCH- 33 pgMCHC- 35.8%RDW- 17.6RBC count- 2.97 millions/cumm
Prothrombin timeProthrombin time- 16 secINR- 1.11
Serum electrolytesSodium- 133 mEq/LPotassium- 3 mEq/LChloride- 94 mEq/L
Serum creatinineSerum creatinine- 0.8 mg/dl
APTTAPTT test- 32 sec
SAAGSerum albumin- 3 gm/dlAscitic albumin- 0.34 gm/dlSAAG- 2.66
Ultrasound
Chest Xray
Provisional diagnosis:Decompensated chronic liver disease with ascites
Treatment:1. Inj PAN 40 mg IV/OD2. Inj LASIX 40mg IV/BD3. Tab Spiranolactone 50mg/ BD4. Inj Thiamine 1 amp in 100 ml NS IV/ TID5. Syrup lactulose 15 ml/ TID6. Abdominal girth charting 4th hourly7. Fluid restriction <1L/ day8. Salt restriction <2g/ day
Ascitic fluid was tapped twice- on 2nd June 2022 & 6th June 2022
Total count- 7200 cells/cumm
Neutrophils- 49%
Lymphocyes- 40%
Eosinophils- 1%
Monocytes- 10%
PCV- 27.4 vol%
MCH- 33 pg
MCHC- 35.8%
RDW- 17.6
RBC count- 2.97 millions/cumm
Prothrombin time
Prothrombin time- 16 sec
INR- 1.11
A 40 years old male, painter by occupation, resident of bhongir has presented to the casualty with the chief complaints of
- Shortness of breath since 7 days
- Chest pain on left side since 5 days
History of presenting illness:
Patient was apparently asymptomatic 7 days ago then he developed shortness of breath which is insidious in onset and gradually progressive from grade 1 to grade 2 according to MMRC
It is aggravated on exertion and postural variation when he lies on his left side and is relieved on rest and sitting position
It was associated with pain which was insidious in onset and gradually progressive and is of pricking type
It is non radiating type and no aggravating and relieving factors
It is not associated with fever, wheezing, palpitations, chest tightness, cough and haemoptysis
Daily routine
Past history:
No history of similar complaints in the past
He is a known case of diabetes mellitus 3 years back and is on medication- Metformin 500mg, Glimiperide 1 mg
Not a known case of Hypertension, asthma, epilepsy and TB
No previous surgical history
Personal historyDiet- MixedAppetite- Decreased since 7 daysBowel and bladder movements- RegularSleep- AdequateAddictions-Patient is a chronic smoker since 20 years- 5 cigarettes/day, but stopped 3 years agoAlcohol - Consuming whisky since 20 years- 90 ml each time, but stopped 3 years agoNo history of drug or food allergies
Family historyNo similar complaints in the family
General examinationDone after obtaining consent, in the presence of attendant with adequate exposurePatient is conscious, coherent, cooperative and well oriented to time, place and personPatient is well nourished and moderately built icterus is positivePedal edema- present- bilateral pitting type
No history of pallor, cyanosis, clubbing and lymphadenopathy
VitalsTemperature- AfebrileBlood pressure- 120/80 mm of HgPulse rate- 78 bpmRespiratory rate- 45 cpmSpO2- 91% at room air
Local examination:Respiratory system examination:
InspectionShape of chest is ellipticalB/L asymmetrical chestTrachea is in central positionExpansion of chest- Right normal; Left decreasedUse of accessory muscles seen (Neck muscles are used)
PalpationAll inspectory findings are confirmedNo local rise of temperature Trachea is deviated to right
Measurements:AP- 24 cmsTransverse- 28 cmsRight hemithorax- 42 cmsLeft hemithorax- 40 cmsCircumferental- 82 cms
Tactile vocal fremitus- Decreased on left side ISA, InfraSA, AA, IAA
PercussionDull note present in left side ISA, InfraSA, AA, IAA
AuscultationB/L air entry present, vesicular breath sounds are heardDecreased intensity of breath sounds in left SSA, IAAAbsent breath sounds in left ISA
Cardiovascular system examination:S1, S2 sounds are heardNo murmursJVP normalApex beat normal
Perabdominal system examination:Soft, non tenderNo organomegalyBowel sounds heardNo guarding, rigidity
Central nervous system examination:No focal neurological deficitsGait- normalReflexes- normal
Provisional diagnosis:Left sided pleural effusion with diabetes mellitus since 3 years
Investigations:FBS- 213 mg/dlHbA1C- 7%
Hb- 13.3mg/dlTC- 5600 cells/cummPLT- 3.57
Serum electrolytesNa- 135 mEq/LK-4.4 mEq/LCl- 97 mEq/L
Serum creatinineSerum creatinine- 0.8 mg/dl
LFTTB- 2.44 mg/dLDB- 0.74 mg/dLAST- 24 IU/LALT- 09 IU/LALP- 167 IU/LTP- 7.5 gm/dLALB- 3.29 gm/dL
Serum LDHSerum LDH- 318 IU/L
Blood ureaBlood urea- 21 mg/dL
Pleural fluidProtein-5.3 mg/dLGlucose-96 mg/dLLDH- 740IU/LTC- 2200DC- 90% lymphocytes10% neutrophils
According to lights criteria (To know if the fluid is transudative or exudative)
NORMAL:Serum Protein ratio: >0.5Serum LDH ratio: >0.6LDH>2/3 upper limit of normal serum LDHProteins >30gm/L
My Patient:Serum protein ratio:0.7Serum LDH: 2.3
INTERPRETATION: As 2 values are greater than the normal we consider as an EXUDATIVE EFFUSION.
(confirmation after pleural fluid c/s analysis)
Chest X-ray
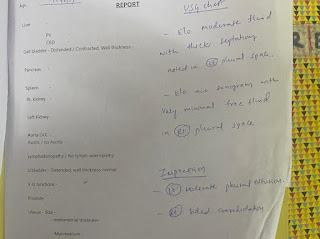
USG
ECG
2D EchoMedication- O2 inhalation with nasal prongs with 2-4 lt/min to maintain SPO2 >94%
- Inj. Augmentin 1.2gm/iv/TID
- Inj. Pan 40mg/iv/OD
- Tab. Pcm 650mg/iv/OD
- Syp. Ascoril-2tsp/TID
- DM medication taken regularly
Advice- High Protein diet
- 2 egg whites/day
- Monitor vitals
- GRBS every 6th hourly
NORMAL:
Serum Protein ratio: >0.5
Serum LDH ratio: >0.6
LDH>2/3 upper limit of normal serum LDH
Proteins >30gm/L
My Patient:
Serum protein ratio:0.7
Serum LDH: 2.3
INTERPRETATION: As 2 values are greater than the normal we consider as an EXUDATIVE EFFUSION.
(confirmation after pleural fluid c/s analysis)
(confirmation after pleural fluid c/s analysis)
Chest X-ray
USG
ECG
2D Echo
Medication
- O2 inhalation with nasal prongs with 2-4 lt/min to maintain SPO2 >94%
- Inj. Augmentin 1.2gm/iv/TID
- Inj. Pan 40mg/iv/OD
- Tab. Pcm 650mg/iv/OD
- Syp. Ascoril-2tsp/TID
- DM medication taken regularly
Advice
- High Protein diet
- 2 egg whites/day
- Monitor vitals
- GRBS every 6th hourly
.jpg)

















Comments
Post a Comment