1701006067 CASE PRESENTATION
LONG CASE
30 years old female, who is HOUSEWIFE by occupation resident of nalgonda
came to the opd with the CHEIF COMPLAINT of
Abdominal pain since 7 days
shortness of breathe since 4 days
pedal edema since 4 days
facial puffiness since 4 days.
HISTORY OF PRESENT ILLNESS:
Patient was apparently asymptomatic 12 months back
then she developed
Abdominal pain : pain since 7 days which started suddenly and burning type of pain In epigastric region No aggravating and reliving factors
Breathlessness:
shortness of breathe since 4 days which is of grade 4 and associated with profuse sweating.
SOB: insidious in onset gradually progressed to grade 4 not associated with change in position no aggravating and relieving factors
Abdominal pain : pain since 7 days which started suddenly and burning type of pain
In epigastric region
No aggravating and reliving factors
PEDAL EDEMA:
She complaints of pedal edema since 4 days which is of pitting type. She had similar edema episodes before this one month which were resolving and reappearing and this time it is not resolved for 1 month.
She also developed facial puffiness
No history of FATIGUE
no history of COUGH, HAEMOPTYSIS
No history of DYSPHAGIA, HOARSENESS OF VOICE
No history of HIGH ARCHED PALATE, CHEST DEFORMITY
No history of RECURRENT RESPIRATORY TRACT INFECTIONS, FEVER, SORE THROAT, CLUBBING, SPLINTER HAEMORRHAGE
No history of FEVER, JOINT PAINS
PAST HISTORY:
She is diagnosed as Gestational HYPERTENSION 12 years back for first pregnancy (after 4th child she discontinued use of anti hypertensive drugs)
She is a not a known case of diabetes, asthma, epilepsy, hyperthyroidism, COPD
No history of blood transfusion
no history of allergy
MARTIAL HISTORY:
Age of menarche 12 year
Marital History:
Age of marriage 18 years
It is a nonconsanguinous marriage
She has 4 children
( in 2011 first child(girl )- normal vaginal delivery -diagnosed as HYPERTENSION
In 2012 second child(girl)- normal vaginal delivery
In 2014 third child(girl) - normal vaginal delivery
In 2015 fourth child(girl)- normal vaginal delivery -she also had episode of Dyspnea of grade 3 (not get attention to symptoms)
FAMILY HISTORY:
father and mother are known case of HYPERTENSION since 6years
PERSONAL HISTORY:
DEIT: mixed
APPETITE: loss of appetite
BOWEL :normal
BLADDER: DECREASED URINE OUTPUT
SLEEP: INadequate
ADDICTIONS: no addictions
GENERAL EXAMINATION:
A 30 year old patient, who is moderately built and well nourished is CONSCIOUS, COHERENT, COOPERATIVE, AND COMFORTABLY LYING ON BED, well oriented to TIME, PLACE AND PERSON.
THERE IS PALLOR
NO icterus
NO cyanosis
No koilonychias
No generalized lymphadenopathy and
No pedal edema
Vitals:
Temperature: a febrile
Pulse: 92/ min
Blood pressure: 150/90 mmHg
Respiratory rate : 34 cpm
SYSTEMIC EXAMINATION:
RESPIRATORY SYSTEM
Patient examined in sitting position
INSPECTION
oral cavity- Normal ,nose- normal ,pharynx-normal
Shape of chest - normal
Chest movements : bilaterally symmetrically reduced
Trachea is central in position & Nipples are in 4th Intercoastal space
APEX IMPULSE VISIBLE IN 6TH INTERCOASTAL SPACE
PALPATION
All inspiratory findings are confirmed
Trachea central in position
Apical impulse in left 6 thICS,
Chest movements bilaterally symmetrical reduced
Tactile and vocal fremitus REDUCED on both sides in infra axillary and infra scapular region
PERCUSSION
DULL IN BOTH SIDES in infra axillary and infra scapular region
AUSCULTATION
DECREASED ON BOTH SIDE in infra axillary and infra scapular region
BRONCHIAL sounds are heared -REDUCED
CARDIOVASCULAR SYSTEM
JVP -raised
Visible pulsations: absent
Apical impulse : shifted downward and laterally 6th intercostal space
Thrills -absent
S1, S2 - heart sounds MUFFLED
PERICARDIAL RUB-PRESENT
ABDOMEN EXAMINATION:
INSPECTION
Shape : distended
Umbilicus:normal
Movements :normal
Visible pulsations :absent
Skin or surface of the abdomen : normal
PALPATION
Liver is not palpable
PERCUSSION- dull
AUSCULTATION :bowel sounds heard
Investigations
HIV TEST
HBSAG
CBP
BLOOD GROUPING
RFT
SERUM IRON
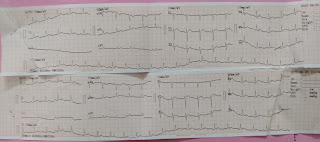
ECG
BACTERIAL CULTURE
2D ECHO
DIAGNOSIS:
IT IS A CASE OF CHRONIC KIDNEY DISEASE ON MAINTENANCE OF HEMODIALYSIS
TREATMENT
INJ. MONOCEF 1gm/IV/BD
INJ. METROGYL 100ml/IV/TID
INJ PAN 40mg/IV/OD
INJ. ZOFER 4mg/iv/SOS
TAB. LASIX 40mg/PO/BD
TAB. NICORANDIL 20mg/PO/TID
INJ. BUSOCOPAN /iv/stat
Add on
TAB. OROFER PO/BD
TAB. NODOSIS 500mg/PO/TID
INJ.EPO 4000 ml/ weekly
TAB. SHELLCAL/PO/BD
DIALYSIS (HD)
INJ.KCL 2AMP IN 500 ml NS over 5min
--------------------------------------------------------------------------------------------------------------------------------------
SHORT CASE
55 YEAR OLD MALE, WHO IS FARMER BY OCCUPATION RESIDENT OF NALGONDA
Came to the opd with the CHIEF COMPLAINTS of
weakness of lower limbs since 4days
VIEW OF THE CASE :
HISTORY OF PRESENT ILLNESS
Patient was apparently asymptomatic 4 months back when he developed pain in the right hip region, which was insidious in onset and intermittent at the beginning. Aggrevated on movement and relieved on rest and medication.
He went to the hospital 2 months ago when the pain progressed and became continuous, and was diagnosed with avascular necrosis of the femur due to a trauma to the hip one year ago.
medications:
Tab.Gabapentin&Nortryptyline
Tab.pantoprazole&Domeperidone
Tab.ETORICOXIN
THIOCOLCHICOSIDE (4mg)
Tab.METHYL COBALAMIN,Biotin
TAB.FERROUS ASCORBATE,
FOLIC ACID And ZINC TABLETS.
4 days ago, patient developed weakness in the lower limb which progressed upto the hip.
He was taken to the hospital and was prescribed medications. On starting the medication, the weakness worsened.
The next morning, patient required ASSISTANCE to WALK and SIT up, BUT FEED HIMSELF. The weakness progressed so that by the evening he was UNABLE to FEED HIMSELF. He only RESPONDED if CALLED to REPEATEDLY
NOT ASSOCIATED WITH SLURRING OF SPEECH
The weakness was not associated with loss of consciousness, drooping of mouth, seizures, tongue bite or frothing of mouth, difficulty in swallowing.
No complaints of any headache, vomitings, chest pain, palpitations and syncopal attacks.
No shortness of breath, orthopnea, paroxysmal nocturnal dyspnea, abdominal pain or burning micturition.
PAST HISTORY:
No similar episodes in the past.
Patient is a known case of diabetes since 12 years. He is on insulin therapy
He was hospitalized, 4 years ago with low blood sugar, and was admitted for 10 days. He presented with altered mental status.
No history of hypertension, tuberculosis, epilepsy, asthma, thyroid and CAD.
No surgical history.
PERSONAL HISTORY:
Diet: Mixed
Appetite: Normal
Sleep: Adequate
Bowel and Bladder: Regular
No allergies
Addictions;
ALCOHOL
Started alcohol intake 25 years back, and stopped 12 years when diagnosed with diabetes. He used to binge drink alcohol for 10 days continuously every month and then used to stop for 20 days. Cycle repeats every month. Now, consumed alcohol only on special occasions, doesn't exceed 90ml.
SMOKING
Started smoking beedis, one a day, 10 years ago.
Stopped 4 years ago when he went into a hypoglycemic episode, but has resumed one year ago.
FAMILY HISTORY:
No similar history in family.
GENERAL EXAMINATION
Patient is examined in a well lit room after taking informed consent.
Patient is conscious, COHERENT and cooperative.
He is moderately built and moderately nourished.
Pallor: Present
Icterus: absent
Cyanosis: absent
Clubbing: absent
Generalized Lymphadenopathy: absent
Edema: Absent
Vitals:
TEMPERATURE AFEBRILE
Blood Pressure: 124/72 mmHg
RESPIRATORY RATE 17 CPM
PULSE RATE 70 BPM
CRANIAL NERVE EXAMINATION
4a) HIGHER MENTAL FUNCTIONS
conscious
• oriented to person and place
• memory - able to recognize their family members and recall recent events
• Speech - no deficit
4b) CRANIAL NERVE EXAMINATION:
I- Olfactory nerve- sense of smell present
II- Optic nerve- direct and indirect light reflex present
III- Oculomotor nerve, IV- Trochlear and VI- Abducens- no diplopia, nystagmus or ptosis
V- Trigeminal nerve- Masseter, temporalis and pterygoid muscles are normal. Corneal reflex is present.
VII- Facial nerve- face is symmetrical, unable to do forehead wrinkling, left nasolabial fold prominent than right.
VIII- Vestibulocochlear nerve- no hearing loss
IX- Glossopharyngeal nerve. X- Vagus- uvula not visualised
XI- Accessory nerve- sternocleidomastoid contraction present
XII- Hypoglossal nerve- Movements of tongue are normal, no fasciculations, no deviation of tongue
MOTOR SYSTEM
ATTITUDE - right lower limb flexed at knee joint
REFLEXES
Right Left
Biceps 2+ 2+
Triceps 2+ 2+
Supinator 2+ 2+
Knee 2+ 2+
Ankle 2+ 2+
SUPERFICIAL reflexes and DEEP reflexes are PRESENT , NORMAL
MUSCLES POWER:
RIGHT LEFT
UPPER LIMB
ELBOW - Flexor 5/5 5/5
- extensor 5/5 5/5
WRIST - Flexor 5/5 5/5
- extensor 5/5 5/5
HAND GRIP 5/5 5/5
LOWER LIMB
HIP - Flexors 5/5 5/5
- extensors 5/5 5/5
KNEE - Flexors 5/5 5/5
- Extensors 5/5 5/5
ANKLE - DF 5/5 5/5
- PF 5/5 5/5
EHL 5/5 5/5
FHL 5/5 5/5
Right Left
BULK
Arm
Forearm 19cm 19cm
Thigh 42cm. 42cm
Leg 28cm. 28cm
TONE
Upper limbs N N
Lower limbs N N
Gait is normal
No involuntary movement
SENSORY SYSTEM - all sensations ( pain, touch, temperature, position, vibration sense) are normal
ATTITUDE - right lower limb flexed at knee joint
TONE - Normal on right side
Normal tone on left side
Bulk - Rt Lt.
Arm: cm cm
Forearm 19cm 19cm
Thigh 42 cm 42cm
Leg 28cm 28cm
CARDIOVASCULAR SYSTEM:
S1 S2 heard, no murmurs
RESPIRATORY SYSTEM:
Bilateral air entry present, normal vesicular breath sounds, no added sounds
GASTROINTESTINAL SYSTEM:
Soft, non-tender, no organomegaly
INVESTIGATION
ECG
TREATMENT
on day 1
1) tab ecospirin 70mg OD
2) tab atorvas 10mg OD
3) inj NS, RL at 70ml/hr
4) syrup potchlor 15ml/po/tid
5) normal oral diet
6) inj HAI - TID
7) 2 amp KCL in 500ml NS slowly over 4-5 hrs
On day 2
1) tab ecospirin 70mg OD
2) tab atorvas 10mg OD
3) inj NS, RL at 70ml/hr
4) syrup potchlor 15ml/po/tid
5) normal oral diet
6) inj HAI - TID
7) proteolytic enema
8) syrup cremaffine
9) tab spironolactone
On day 3
1) tab ecospirin 70mg OD
2) tab atorvas 10mg OD
3) inj NS, RL at 70ml/hr
4) syrup potchlor 15ml/po/tid
5) normal oral diet
6) inj HAI - TID
7) proteolytic enema
8) syrup cremaffine plus 15ml/po/od
9) tab spironolactone 25mg/po/od
10) tab azithromycin 500mg OD
11) high protein diet
On day 4
1) tab ecospirin 70mg OD
2) tab atorvas 10mg OD
3) inj NS, RL at 70ml/hr
4) syrup potchlor 15ml/po/tid
5) normal oral diet
6) inj HAI - TID
7) tab ultracet QID
8) syrup cremaffine plus 15ml/po/od
9) tab spironolactone 25mg/po/od
10) tab azithromycin 500mg OD
11) high protein diet
On day 5
1) tab ecospirin 70mg OD
2) tab atorvas 10mg OD
3) inj NS, RL at 70ml/hr
4) syrup potchlor 15ml/po/tid
5) normal oral diet
6) inj HAI - TID
7) tab ultracet 1/2 po/ QID
8) syrup cremaffine plus 15ml/po/od
9) tab spironolactone 25mg/po/od
10) tab azithromycin 500mg OD
11) high protein diet






































Comments
Post a Comment