1701006068 CASE PRESENTATION
LONG CASE
A 70-year-old male has presented to the hospital on 06 June 2022 with the chief complaints of
- slurring of speech
- difficulty in walking
- weakness of right upper and lower limbs
since 9 days
HISTORY OF PRESENT ILLNESS:
The patient was leading a peaceful life with his wife. He would wake up every day at about 6am, freshen up, have breakfast and do his daily chores like grazing the cattle till the afternoon. He would then have lunch and take a nap till evening. He then hung out with the neighbours, had dinner and rested for the day. This was his routine.
1st episode: Patient had been asymptomatic until 3 years ago when he suddenly acquired weakness in his right upper and lower limbs, with no slurring of speech. After being treated, he was able to recover.
2nd episode: He suffered a second episode of abrupt onset weakening of the right upper and lower limbs a year ago, which was accompanied by drooping of the mouth and saliva dribbling. He was treated for it again and fully healed.
3rd episode: He developed weakness of the left upper and lower limbs 9 days ago. He first was not able to walk then eat and then developed speech abnormality. He then went to an RMP and it was found that his blood pressure was high and advised the patient to go to the hospital. These were sudden in onset and progressed gradually.
- not a known case of diabetes, asthma, epilepsy, or TB.
- diagnosed with hypertension 10 months ago and has been using atenolol 25mg since.
- married
- normal appetite
- takes vegetarian diet predominantly
- bowel movements: regular
- micturition is normal
- no known allergies
- addictions: alcohol abstinence for 5 years.
Done after obtaining consent, in a well-lit room, in the presence of an attendant, with adequate exposure. The patient is conscious, incoherent, cooperative, well-nourished, and well-oriented to time, but not oriented to place and person.
- No pallor icterus, Cyanosis, Koilonychia, Generalised Lymphadenopathy, Pedal oedema and clubbing
- Slight muscle wasting in the right upper arm is observed
VITALS
- Temperature - afebrile
- Pulse rate- 70 bpm
- BP- 140/80 mm Hg
- Respiratory rate- 16/min
2. Respiratory system:
- Bilateral air entry present
- Normal vesicular breath sounds heard
4. CNS:
Dominance - Right-handed
4a) Higher mental functions
- conscious and cooperative but incoherent
- oriented to time, but not oriented to place and person.
- memory- not able to recognize family members
- Speech - only comprehension, no fluency, no repetition
- I- Olfactory nerve- sense of smell present
- II- Optic nerve- direct and indirect light reflex present
- III- Oculomotor nerve, IV- Trochlear and VI- Abducens- no diplopia, nystagmus or ptosis
- V- Trigeminal nerve- Masseter, temporalis and pterygoid muscles are normal. Corneal reflex is present.
- VII- Facial nerve- face is symmetrical, unable to do forehead wrinkling, left nasolabial fold prominent than right.
- VIII- Vestibulocochlear nerve- no hearing loss
- IX- Glossopharyngeal nerve. X- Vagus- uvula not visualised
- XI- Accessory nerve- sternocleidomastoid contraction present
- XII- Hypoglossal nerve- Movements of tongue are normal, no fasciculations, no deviation of tongue
- crude touch present present
- fine touch absent present
- pain absent present
- vibration absent present
- temperature absent present
- stereognosis- absent present
- 2 pt discrimination- absent present
- graphaesthesia- absent present
CBP
- Hemoglobin- 12.6 gm/dl (N)
- PCV- 35.2 % (N)
- TLC- 8600/ cumm (N)
- RBC- 4.33 million/cumm (N)
- Platelets- 2.58 lakhs/ml (N)
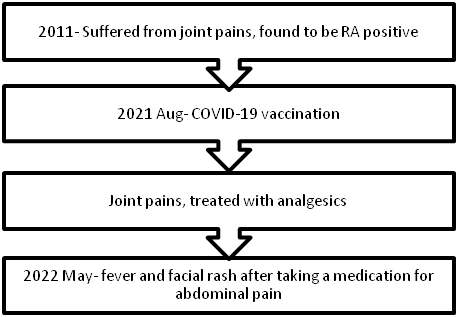
TIMELINE OF EVENTS:
A 47-year-old male has presented to the hospital on 02 June 2022 with the chief complaints of
- fever
- rash over the face
HISTORY OF PRESENT ILLNESS:
The patient was apparently asymptomatic ten years ago then she developed joint pains in both knees and ankles, then both hands. There was swelling, and stiffness in the morning for around 15 minutes, with movement restrictions. The patient was treated at a private hospital and was diagnosed as RA POSITIVE and was prescribed diclofenac.
- Patient had a history of vision deterioration and began wearing spectacles at the age of 15 years, but the loss of eyesight was gradual, progressive, and painless, and he was declared legally blind. No relevant drug or trauma history .
- not a known case of hypertension , diabetes, asthma, epilepsy, TB.
- married
- normal appetite
- takes mixed diet
- bowel movements: regular
- micturition is normal
- no known allergies
- addictions: none
Done after obtaining consent. The patient is conscious, incoherent, cooperative, well-nourished, and well -oriented to time, but not oriented to place and person.
Pallor: present
- No icterus, cyanosis, clubbing,lymphadenopathy, edema.
VITALS
- Temperature - afebrile
PULSE:86BPM
- BP:120/80mm hg
- RR:16cpm
inspection: shape of the chest is normal
no visible neck veins
No rise in JVP
palpation: all inspectory findings are confirmed
apex beat normal at 5th ics medial to mcl
no additional palpable pulsations or murmurs
percussion: showed normal heart borders
auscultation: S1 S2 heard no murmurs or additional sounds
2. Respiratory system:
inspection: normal chest shape bilaterally symmetrical, mediastinum central
no scars, Rr normal, no pulsations
palpation: Insp findings are confirmed
percussion: normal resonant note present bilaterally
auscultation: normal vesicular breath sounds heard
3. GIT:palpation - inspectory findings are confirmed
no organomegaly, non tender and soft
percussion- normal resonant note present, liver border normal
auscultation-normal abdominal sounds heard, no bruit present
4. CNS:
Higher mental functions
- conscious and cooperative coherent
- oriented to time, place and person.
- memory- recent and immediate memory intact
CRANIAL NERVE EXAMINATION
2nd cranial nerve. Right. Left
Visual acuity. Counting fingers
Counting fingers postive
Direct light reflex present. Present
Indirect light reflex present. Present
Perception of light. Present. Present
Remaining cranial nerves normal.
SENSORY :
touch, pressure, vibration, and proprioception are normal in all limbs
MOTOR-: normal tone and power
reflexes: RT LT
BICEPS ++ ++
TRICEPS ++ ++
SUPINATOR ++ ++
KNEE ++ ++
CBP
- Hemoglobin- 6 gm/dl
- PCV- 21 %
- TLC- 8200/ cumm
- RBC- 2.5 million/cumm
- Platelets- 1.32 lakhs/ml
1.INJ PIPTAZ 4.5 gm IV/ TID.
2.INJ METROGEL100 ML IV/TID
3.INJ NEOMOL1GM/IV/SOS
4.TAB CHYMORAL FORATE PO/TID
5.TAB PAN 40 MG PO/ OD.
6.TAB TECZINE10 MG PO/OD
7.TAB OROFERPO/OD.
8.TAB HIFENAC-P PO/OD
9HYDROCOTISONE cream 1%on face for 1week.











Comments
Post a Comment