LONG CASE
A 46 year old male came to the casualty with complaints of
Burning micturition since 10days
Vomitings since 2 days
Drowsiness since 1 day
History of present illness
Past History:
No history of previous UTI
He is not a known case of Hypertension, Coronary artery disease, asthma, TB
Personal History:
Appetite- normal
Diet- mixed
Regular bladder and bowel movements
Burning micturition since 10 days(18/05/22)
Addictions: consumes alcohol occasionally but stopped since 1 yr.
General Examination:
Moderately built and nourished.
Pallor present
No- icterus,cyanosis,clubbing,koilonychia, lymphadenopathy
No visible signs of dehydration
Vitals at admission:
BP: 110/80 mm of hg
HR: 98bpm
RR: 18cpm
Temperature: 101 degree farenheit
SpO2: 98% on RA
GRBS: 124 mg/dL





Construction apraxia ( reference picture)
Systemic Examination:
CVS: S1S2 heard, No murmurs
RS: Bilateral air entry is present.
Normal vesicular breath sounds are heard
P/A
Soft, non tender.
No scars,engorged veins ,sinuses,swelling
No visible gastric peristalsis
No renal angle fullness
CNS:
Patient is having altered sensorium
Reflexes:
Biceps,Triceps,Supinator,Knee,Ankle,Plantar-All are normal
Power- 5/5 in both upper and lower limbs
Tone- nomal in both upper and lower limbs
Meningeal signs are not seen
Investigations:
On admission
19.5.22
1) Complete blood picture
2) Complete urine examination
3) Urine for ketone bodies:
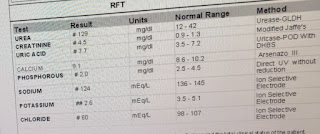
4)Renal function tests:
5) Liver function tests:
6) X-ray KUB
20.05.22
1)LDH- 192
2) 24Hr urine creatinine
3) 24Hr urine proteins
21.5.22
Hemoglobin- 6.8g%
TLC- 22,500cells/cumm
Platelets- 1.4lakhs/cu.mm
Urea- 155mg/dl
Creatinine- 4.7
Uric acid- 7.1
Phosphorus- 2.0
Sodium- 126
Potassium- 2.6
Chloride- 87
22.5.22
Hemoglobin- 7.2
TLC- 17,409
Platelet count- 1.5
Urea- 162
Uric acid- 5.0
Sodium- 125
Chloride- 88
23.05.22
1) Bacterial culture and sensitivity report
Culture report: Klebsiella Pneumonia positive
24.05.22
1) 2D Echo:
2) Bacterial culture and sensitivity report

Patient Complained of Sudden diminision of vision in right eye
Sent for ophthalmologic examination
Diagnosed as secondary angle closure glaucoma
Treated with timolol bd for 1 week and glycerol 5times daily for 1 week
25.5.22
27.5.22
Hb- 7
TLC- 22,000
Platelet count- 26,000
Urea- 144
Creatinine - 4.8
Uric acid-9.1
Phosphorus- 4.8
Sodium- 135
Potassium- 4.3
Chloride- 98
Fasting blood sugar- 149
29.5.22
Hb- 6.4
TLC- 14,700
Platelet count- 6000
Urea - 149
Creatinine- 4.4
Uric acid- 9.2
30.05.22
07.06.22
Provisional Diagnosis:
Right emphysematous pyelonephiritis and left acute pyelonephiritis and encephalopathy secondary to sepsis.
H/o of Type 2 Diabetes Mellitus since 10years
Treatment:
INJ. MEROPENEM 500mg IV BD
INJ. ZOFER 4mg IV TID
INJ. RANTAC 50mg IV OD
INJ. KCl 2 Amp in 500 mL NS over 4.5 hrs infusion
IV Fluids- NS,RL @ 100 mL/hr
SYP. POTCHLOR 10 mL in 1 glass of water TID
SYP. MUCAINE GEL 10 mL PO TID
7 point profile
BP/HR/RR/SpO2 charting
Temp charting 4th hrly
RT feeds- 2nd hrly 100 mL water
INJ. COLISTIN 2.25 MU IV OD
--------------------------------------------------------------------------------------------------------------------------------------
SHORT CASE
A 50 years old patient, who is a farmer by occupation, resident of pochampally has presented to the casualty on 02-06-2022 with the chief complaints of
- Abdominal distension since 8 days
- Pain in the abdomen since 8 days
- Pedal edema since 6 days
History of present illness:
Patient was apparently asymptomatic 6 months back, then he developed jaundice for which he was treated by a local private practitioner.
15 days back he consumed more than the usual amount of alcohol following which he started experiencing some discomfort and since 4 days developed abdominal distension which was insidious in onset, gradually progressive and progressed to present size.
It is associated with pain in epigastrium and right hypochondrium.
Patient complained of bilateral pedal edema of grade 2 below the kneee since 3 days which was insidious in onset, gradually progressive, pitting type, increased as the day progressed and had no relieving factors.
Associated symptoms : shortness of breath since 3 days.
No history of nausea and vomiting.
No history of chest pain, exercise intolerance.
No history of evening rise of temperature, cough, night sweats.
No history of hematemesis, dilated veins, hemorrhoids, melena.
No history of facial puffiness, generalized edema.
PAST HISTORY :
No history of similar complaints in the past.
Patient is not a known case of Diabetes mellitus, Hypertension, Tuberculosis, Asthma, Epilepsy, Thyroid disease.
There is no history of blood transfusion or hospital admission.
PERSONAL HISTORY :
Diet : Mixed
Appetite : Decreased
Sleep : Adequate
Bowel and bladder movements : Urine frequency is reduced since 2 days and patient has an history of constipation.
Addictions : Patient is a chronic smoker and smoked 4-5 bidis per day since past 30 years (Pack years=Number of cigarettes x years of smoking/20; 5x30/20 = 7.5)
Patient consumes alcohol occasionally (whenever he gets tired from work) - 90 ml of whiskey (previously he was a chronic alcoholic but stopped consuming regularly 6 months back).
Patient consumes toddy occasionally
FAMILY HISTORY :
No significant family history.
HISTORY OF ALLERGIES :
No known food or drug allergies.
GENERAL PHYSICAL EXAMINATION :
Patient is conscious, coherent, co-operative and well-oriented to time, place and person.
Patient is moderately built and is moderately nourished.
There is pedal edema of grade 2.
Icterus is present.
There is no pallor, cyanosis, clubbing, lymphadenopathy.
Vitals :
Temperature : Afebrile
Pulse rate : 90 bpm, regular, normal volume.
Respiratory rate : 22 cpm
Blood pressure : 130/90 mm Hg Right arm in sitting position
GRBS : 90 mg/dl
O2 saturation : 98%
SYSTEMIC EXAMINATION :
Per abdomen :
On Inspection :
Abdomen appears to be distended and the umbilicus is everted.
Skin is smooth and shiny.
There are no abnormal swellings, discoloration, scars, sinuses, fistulae, venous dilatations.
On palpation :
There is no local rise of temperature.
Tenderness is present in the epigastrium.
No hepatomegaly. No splenomegaly.
Guarding is present.
Rigidity is absent.
Kidney not palpable.
On Percussion :
Tympanic note is heard on the midline of abdomen and a dull note is heard on the flanks in supine position.
Shifting dullness : Positive
Liver span could not be detected.
No renal angle tenderness.
Auscultation :
Bowel sounds are decreased.
No bruits could be heard.
Cardiovascular System : S1, S2 heard
Respiratory System : Normal vesicular breath sounds heard
Central Nervous System : Conscious; Speech normal ; Motor and sensory system examination is normal, Gait is normal.
INVESTIGATIONS :
1. Hemogram :
Hemoglobin : 9.8 g/dl
TLC : 7,200
Neutrophils : 49%
Lymphocytes : 40%
Eosinophils : 1%
Basophils : 0%
PCV : 27.4%
MCV : 92.3 fl
MCH : 33 pg
MCHC : 35.8%
RDW-CV : 17.6%
RDW-SD : 57.8 fl
RBC count : 2.97 millions/mm3
Platelet count : 1.5 lakhs/mm3
Smear : Normocytic normochromic anemia
2. Serology :
HbsAg : Negative
HIV : Negative
3. ESR :
15mm/1st hour
4. Prothrombin time : 16 sec
5. APTT : 32 sec
6. Serum electrolytes :
Sodium : 133 mEq/L
Potassium : 3 mEq/L
Chloride : 94 mEq/L
7. Blood Urea : 12 mg/dl
8. Serum Creatinine : 0.8 mg/dl
9. LFTs :
Total Bilirubin : 2.22 mg/dl
Direct Bilirubin : 1.13 mg/dl
AST : 147 IU/L
ALT : 48 IU/L
ALP : 204 IU/L
Total proteins : 6.3 g/dl
Serum albumin : 3 g/dl
A/G ratio : 0.9
10. Ascitic fluid :
Protein : 0.6 g/dl
Albumin : 0.34 g/dl
Sugar : 95 mg/dl
LDH : 29.3 IU/L
SAAG : 2.66 g/dl
11. Ascitic Fluid Cytology :
12. Ascitic fluid culture and sensitivity report :
13. Ultrasound :
Coarse echotexture and irregular surface of liver - Chronic liver disease
Gross ascites
Gallbladder sludge
14.X-ray
PROVISIONAL DIAGNOSIS :
Decompensated Chronic liver disease with ascites most likely etiology is alcohol.
TREATMENT :
Drugs :
1. Inj. Pantoprazole 40 mg IV OD
2. Inj. Lasix 40 my IV BD
3. Inj. Thiamine 1 Amp in 100 ml IV TID
4. Tab. Spironolactone 50 mg BB
5. Syrup Lactulose 15 ml HS
6. Syrup Potchlor 10ml PO TID
7. Fluid restriction less than 1L/day
8. Salt restriction less than 2g/day
Ascitic fluid tapping :
Ascitic fluid was tapped twice (2-06-2022 and 6-06-2022)











































Comments
Post a Comment