LONG CASE
A 50 years old gentleman, farmer by occupation, resident of Yadadri Bhuvanagiri district came to the hospital with the following cheif complaints.
CHEIF COMPLAINTS:
- Distension of abdomen since 7 days
- Pain in the abdomen since 4 days and
- Pedal edema since 3 days
HISTORY OF PRESENT ILLNESS:
Patient was apparently asymptomatic 6 months back then he developed jaundice and he was treated for jaundice by a private medical practitioner. After that he was normal till last week.
He developed distension of abdomen 7 days back, which is insidious in onset, gradually progressive, aggravated in last 4 days and progressed to the present size. No aggravating and releiving factors.
He complaints of abdominal pain from last 3 days which is insidious in onset, gradually progressive, in the epigastrium and right hypochondrial regions without any aggravating and releiving factors.
He also complains of swelling in both feet of Grade II since 3 days which is insidious in onset, gradually progressive, pitting type without any aggravating and releiving factors.
NO history of hemetemesis, melena, vomitings, nausea
NO history of bulky stools, black tarry and clay colored stools
NO history of fever with chills and rigor
NO history of anorexia, facial puffiness, generalised edema
NO history of evening rise of temperature, cough, night sweats
NO history of orthopnea, palpitations
NO history of loss of weight
PAST HISTORY:
NO history of similar complaints in the past.
Not a known case of Diabetes, Hypertension, Tuberculosis, Asthma, epilepsy, hypothyroidism/hyperthyroidism, COPD, CAD and blood transfusions.
FAMILY HISTORY:
None of the patient's parents, siblings or first degree relatives have or had similar complaints or any significant comorbidities.
PERSONAL HISTORY:
Appetite: reduced
Diet: mixed
Bladder habits: frequency of urine is reduced since 2 days
Bowel habits: constipation since last 4 days
Sleep: Adequate
Addictions:
- Beedi smoker: for past 30 years. 4-5 beedis per day
Pack years= no. of cigarettes×years of smoking/20
Number of beedis = numbr of cigarettes/4
Therefore,
Pack years = 5/4×30/20
Pack years = 1.88 pack years
- Alcoholic: chronic alcoholic previously
From last one year, occasional alcoholic - consumes 90ml of whiskey
GENERAL PHYSICAL EXAMINATION:
Patient is conscious, coherent and cooperative.
Examined after taking vaild informed consent in a well enlightened room.
Built and nourishment: moderately built and moderately nourished
Pallor: No pallor
Icterus: No icterus
Cyanosis: No cyanosis
Clubbing: No clubbing
Generalised lymphadenopathy: No generalised lymphadenopathy
Pedal edema: Grade II bilateral pedal edema
VITALS:
Temperature: afebrile
Pulse rate: 90bpm, regular rhythm, normal volume
Respiratory Rate: 22 breathes per minute, abdominothoracic type
Blood Pressure: 130/90 mm of Hg in right arm in sitting position
GRBS: 90mg/dl
SpO2: 98% at room air
TREMORS: present
SYSTEMIC EXAMINATION:
PER ABDOMINAL EXAMINATION:
INSPECTION: 9 regions
Shape of the abdomen: globular
Distension of abdomen: distended
Flanks: full
Umbilicus:
Shape: everted
Position: central
Herniations: absent
Discharge: absent
Skin over abdomen: smooth and shiny
No pigmentations, discolorations, scars, sinuses, fistulae, engorged veins, visible pulsations, hernial orifices,
Genitals: normal
PALPATION:
No local rise of temperature
Tenderness: present in the epigastrium region
Hepatomegaly: absent
Splenomegaly: absent
Guarding: present
Rigidity: absent
Renal angle tenderness: absent
No rebound tenderness
No visible peristalsis
FLUID THRILL(with extended legs): POSITIVE
PERCUSSION:
In supine position,
Tympanic note - heard at midline of the abdomen
Dull note - heard at flanks
Shifting dullness: POSITIVE
Liver span : could not be detected
AUSCULTATION:
Bowel sounds: decreased
No bruits
CARDIOVASCULAR SYSTEM-
Inspection-
The chest wall is bilaterally symmetrical
No dilated veins, scars or sinuses are seen
Apical impulse or pulsations cannot be appreciated
Palpation-
Apical impulse is felt in the fifth intercostal space, 1 cm medial to the midclavicular line
No parasternal heave felt
No thrill felt
Percussion-
Right and left borders of the heart are percussed
Auscultation-
S1 and S2 heard, no added thrills and murmurs are heard
RESPIRATORY SYSTEM:
Inspection:
Shape- elliptical
B/L symmetrical ,
Both sides moving equally with respiration .
Palpation:
Trachea - central
Expansion of chest is symmetrical.
Vocal fremitus - normal
Percussion: resonant bilaterally
Auscultation:
bilateral air entry present. Normal vesicular breath sounds heard.
CENTRAL NERVOUS SYSTEM
Higher mental functions :-
Patient is conscious ,coherent and cooperative
Right handed individual
Memory - immediate , short term and long term memory are assessed and are normal
Language and speech are normal
Cranial nerves :- intact
Sensory system :-
Sensation right left
Touch felt felt
Pressure felt felt
Pain
-superficial felt felt
-deep felt felt
Proprioception
-joint position ✔ ✔
-joint movement ✔ ✔
Temperature felt felt
Vibration felt felt
Stereognosis ✔ ✔
Motor system
Right. Left
BULK
Upper limbs. N N
Lower limbs N N
TONE
Upper limbs. N N
Lower limbs. N N
POWER
Upper limbs. 5/5 5/5
Lower limbs 5/5 5/5
Gait :- Normal
Superficial and deep reflexes are elicited
No signs ssuggestive of cerebellar dysfunction
INVESTIGATIONS:
1. HEMOGRAM:
Hemoglobin : 9.8 g/dl
TLC : 7,200
Neutrophils : 49%
Lymphocytes : 40%
Eosinophils : 1%
Basophils : 0%
PCV : 27.4%
MCV : 92.3 fl
MCH : 33 pg
MCHC : 35.8%
RDW-CV : 17.6%
RDW-SD : 57.8 fl
RBC count : 2.97 millions/mm3
Platelet count : 1.5 lakhs/mm3
Smear : Normocytic normochromic anemia
2. Serology :
HbsAg : Negative
HIV : Negative
3. ESR :
15mm/1st hour
4. Prothrombin time : 16 sec
5. APTT : 32 sec
6. Serum electrolytes :
Sodium : 133 mEq/L
Potassium : 3 mEq/L
Chloride : 94 mEq/L
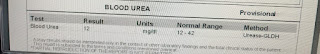
7. Blood Urea : 12 mg/dl
8. Serum Creatinine : 0.8 mg/dl
9. LFT :
Total Bilirubin : 2.22 mg/dl
Direct Bilirubin : 1.13 mg/dl
AST : 147 IU/L
ALT : 48 IU/L
ALP : 204 IU/L
Total proteins : 6.3 g/dl
Serum albumin : 3 g/dl
A/G ratio : 0.9
10. Ascitic fluid :
Protein : 0.6 g/dl
Albumin : 0.34 g/dl
Sugar : 95 mg/dl
LDH : 29.3 IU/L
SAAG : 2.66 g/dl
ASCITIC FLUID CYTOLOGY:
Microscopy:
Cytology smear study shows few scattered lymphocytes, reactive mesothelial cells against a granular eosinophilic proteinaceous background.
No atypical cells are seen.
Impression: negative for malignancy
ASCITIC FLUID CULTURE AND SENSITIVITY REPORT:
ZN staining: No acid fast bacilli seen.
Few epithelial cells with no inflammatory cells seen. No organisms seen.
No growth after 48 hours of aerobic incubation
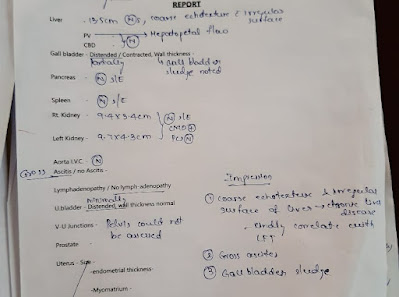
ULTRASONOGRAPHY:
Coarse echotexture and irregular surface of liver - Chronic liver disease
Gross ascites
Gallbladder sludge
ELECTROCARDIOGRAPHY:
CHEST RADIOGRAPHY:
ASCITIC FLUID TAPPING: Done twice
Severity of liver disease:
CHILD-PUGH-TURCOTTE SCORING SYSTEM:
Parameter points asigned
1 2 3
Ascites absent slight moderate
Bilirubin(mg/dl) <2 2-3 >3
Albumin(g/dl) >3.5 2.8-3.5 <2.8
Prothrombin time <4 4-6 >6
Encephalopathy None Grade 1-2 grade 3-4
Interpretation:
Total score: 5-6 well compensated disease
7-9 significant functional compromise
10-15 decompensated disease
In this patient,
Ascites - moderate(3)
Bilirubin- 2.22mg/dl (2)
Albumin - 3g/dl (2)
Prothrombin time- 16 seconds (3)
Encephalopathy- none(1)
Total score: 11
Therfore this patient's liver condition is in Decompensated state.
PROVISIONAL DIAGNOSIS:
This is a case of Decompensated Chronic liver disease with ascites, probably secondary to chronic alcoholism.
TREATMENT:
1. Inj. PANTOPRAZOLE 40 mg IV OD
2. Inj. LASIX 40 my IV BD
3. Inj. THIAMINE 1 Amp in 100 ml IV TID
4. Tab. SPIRONOLACTONE 50 mg BB
5. Syrup. LACTULOSE 15 ml HS
6. Syrup. POTCHLOR 10ml PO TID
7. Fluid restriction less than 1L/day
8. Salt restriction less than 2g/day
----------------------------------------------------------------------------------------------------------------------------------------------------
SHORT CASE
A 40 years old gentleman, painter by occupation, resident of Bhongir presented to the hospital with the following cheif complaints.
CHEIF COMPLAINTS:
- Shortness of breathe since 7 days
HISTORY OF PRESENT ILLNESS:
Patient was apparently asymptomatic 7 days back then he developed shortness of breathe which is insidious in onset, gradually progressive from Grade I to Grade II(MMRC), aggravates on exertion and lying on left side(postural variation), releives on rest and sitting position and not associated with wheeze, cough.
Loss of weight of about 10kgs in last 1 year.
NO history of vomitings, Orthopnoea, PND, edema,
NO history of chest pain, fever, hemoptysis, palpitations,
NO history of recurrent cold or sorethroat
NO history of loss of consciousness, convulsions
NO history of joint pains
PAST HISTORY:
NO history of similar complaints in the past.
He is a known diabetic since 3 years. And he is on oral antidiabetic medications [GLIMIPERIDE 1mg and METFORMIN 500mg]
He is not a known case of Hypertension, asthma, tuberculosis, epilepsy, thyroid disorder, CVD, COPD, blood transfusions
FAMILY HISTORY:
None of the patient's parents, siblings or first degree relatives have or had similar complaints or any significant comorbidities.
PERSONAL HISTORY:
Appetite: loss of appetite
Diet: mixed
Bowel: regular
Bladder : regular
Sleep: Adequate (disturbed sleep drom last 5 days)
Addictions: Alcoholic(90ml/day) since last 20 years but stopped 1 year back
Smoker(3 cigarettes/day) since last 20 years but stopped 1 year back
Pack years= no. of cigarettes×years of smoking/20
Pack years = 3×20/20
Pack years = 3 pack years
GENERAL PHYSICAL EXAMINATION:
Patient is conscious, coherent and cooperative.
Examined after taking a valid informed consent in a well enlightened room.
Built and nourishment: moderately built and moderately nourished
Pallor: No pallor
Icterus: No icterus
Cyanosis: No cyanosis
Clubbing: No clubbing
Generalised lymphadenopathy: No generalised lymphadenopathy
Pedal edema: No pedal edema
VITALS:
Temperature: afebrile
Pulse rate: 139bpm, regular rhythm, normal volume
Respiratory Rate: 45 breathes per minute, abdominothoracic type
Blood Pressure: 110/70 mm Hg measured in right arm in sitting position
GRBS: 201mg/dl
SpO2: 91% at room air
SYSTEMIC EXAMINATION:
RESPIRATORY SYSTEM:
INSPECTION
Shape of the chest: elliptical
Symmetry of the chest: bilaterally symmetrical
Tracheal position : central
expansion of chest: normal on right side and decreased on left side
use of accessory muscles: present
Skin over the chest: normal.
No engorged veins, sinuses, subcutaneous nodules, scars, swellings and pigmentations.
No drooping of shoulders
No crowding of ribs
PALPATION
Inspectory findings confirmed
No tenderness and local rise of temperature.
Tracheal position: central
Chest measurements:
Anteroposterior length: 28cm
Transverse length: 28cm
Right hemithorax: 42cm
Left hemithorax: 40cm
Circumference: 82cm
Tactile vocal fremitus: decreased on left inframammary area, infrascapular area infraaxillary area.
No bony tenderness
PERCUSSION
Dull note heard at the left infraaxillary and infrascapular areas
Liver dullness from right 5th intercostal space
Heart borders are within normal limits
AUSCULTATION
Bilateral air entry present.
Vesicular breath sounds heard.
Decreased intensity of breathe sounds heard in left inframammary area and infrascapular area and absent breathe sounds in left infraxillary area.
No abnormal and adventitious sounds.
Vocal resonance: decreased in left infraaxillary and infrascapular areas.
CARDIOVASCULAR SYSTEM:
First and Second heart sounds heard. No murmers.
CENTRAL NERVOUS SYSTEM:
HIgher mental functions- normal
No focal neurological deficit
No facial asymmetry. All reflexes are normal.
PER ABDOMEN EXAMINATION:
Soft, non tender,
no hepatomegaly and splenomegaly.
INVESTIGATIONS:
BLOOD GLUCOSE AND HBA1C:
FBS: 213mg/dl
HbA1C: 7.0%
HEMOGRAM:
Hb: 13.3gm/dl
TC: 5,600cells/cumm
PLT: 3.57
SERUM ELECTROLYTES:
Na: 135mEq/l
K: 4.4mEq/l
Cl: 97mEq/l
SERUM CREATININE:
Serum creatinine: 0.8mg/dl
LFT:
TB: 2.44mg/dl
DB: 0.74mg/dl
AST: 24IU/L
ALT: 09IU/L
ALP: 167IU/L
TP: 7.5gm/dl
ALB: 3.29gm/dl
LDH: 318IU/L
Blood urea: 21mg/dl
CHEST XRAY:
On the day of admission
Subsequent x rays
After starting treatment
ELECTROCARDIOGRAPHY:
ULTRASONOGRAPHY:
USG Chest:
- Evidence of moderate fluid with thick septations in left pleural space
- Eveidence of air sonogram very minimal fluid in right pleural space
Impression : left moderate pleural effusion and right sided consolidation.
2D ECHOCARDIOGRAPHY:
Large pleural effusion (+)
Good left ventricular systolic function
No RWMA, No Mitral stenosis or atrial stenosis
No mitral regurgitation and aortic regurgitation
No pulmonary embolism or left ventricular clot
No diastolic dysfunction
inferior venacavae size is normal.
NEEDLE THORACOCENTESIS:
-under strict aseptic conditions USG guidance 5%xylocaine instilled 20cc syringe 7th intercoastal space in mid scapular line left hemithorax pale yellow coloured fluid of 400ml of fluid is aspirated diagnostic approach.
PLEURAL FLUID:
Protein: 5.3gm/dl
Glucose: 96mg/dl
LDH: 740IU/L
TC: 2200
DC: 90% lymphocytes
10% neutrophils
ACCORDING TO LIGHTS CRITERIA: (To know if the fluid is transudative or exudative)
Pleural fluid is an exudate if one or more of the following criteria are met.
Parameters:
Pleural fluid protein : Serum Protein ratio: >0.5
Pleural fluid LDH : Serum LDH ratio: >0.6
Pleural fluid LDH>2/3 upper limit of normal serum LDH
Patient:
Pleural fluid protein: Serum protein ratio= 0.7
Pleural fluid LDH : Serum LDH= 2.3
Pleural fluid LDH is greater than 2/3rd of upper limit of normal serum LDH
INTERPRETATION: As 3 values are greater than the normal we consider as an EXUDATIVE EFFUSION.
(confirmation after pleural fluid c/s analysis)
DIAGNOSIS:
This is a case of left sided pleural effusion with Diabetes as comorbidity.
TREATMENT:
Medication:
O2 inhalation with nasal prongs with 2-4 lt/min to maintain SPO2 >94%
Inj. AUGMENTIN 1.2gm/iv/TID
Inj. PANTOPRAZOLE 40mg/iv/OD
Tab. PARACETAMOL 650mg/iv/OD
Syp. ASCORIL-2TSP/TID
DM medication taken regularly
Advice:
High Protein diet
2 egg whites/day
Monitor vitals
GRBS every 6th hourly




































Comments
Post a Comment