LONG CASE
Chief Complaints:-
A 47 year old female tailor by occupation resident of nalgonda came to the OPD with the chief complaints of:
Fever since 3 months
Facial rash since 10 days
HISTORY OF PRESENT ILLNESS:-
Patient was apparently asymptomatic 10 years ago then she developed joint pains first in the both knees and ankles followed by both the hands.There was swelling associated with pain and morning stiffness for about 15mins associated with limitation of movements. For this patient was treated in private hospital and was tested RA POSTIVE and was on diclofenac,remained asymptomatic for 8 months,
Last year at around month of August patient took covid vaccination of one dose following which she developed post vaccination joint pains.
In the month of November patient consulted orthopedic and was given medication and thus relieved from symptoms.
3months back then she developed fever which was Insidious in onset Intermittent on and off not associated with chills and rigor. Relieved on medication . She went to the private hospital but the fever was recurrent associated with abdominal pain came to our hospital 5 days back.
1 month back patient had an episode of loss of consciousness associated with sweating after taking metformin tablet prescribed by local RMP
Patient also had facial rash over the face which increased on exposure to sun. It was a diffuse erythematous lesion and hyperpigmented papules were noted over the bilateral cheek sparing nasolabial folds, following intake of unknown medication for abdominal pain
PAST HISTORY:-
Patient had an history of gradual painless loss of vision since 2011and was certified as blind
Not a known case of diabetes, asthma, Epilepsy ,thyroid tuberculosis and coronary artery disease.
No similar complaints in the family
PERSONAL HISTORY:-
Diet: Mixed
APPETITE: Decreased
SLEEP: Disturbed
BOWEL AND BLADDER MOVEMENTS: Regular
ADDICTIONS: No addiction
GENERAL EXAMINATION:-
Pateint is consious coherent and co operative. Well oriented to time ,place and person,moderately built and moderately nourished and is examined with informed consent.
Pallor: present
No icterus, cyanosis, clubbing,lymphadenopathy, edema.
VITALS:-
PULSE :86BPM
BP:120/80mm hg
RR:16cpm
SPO2:98%at room air
LOCAL EXAMINATION:-
There is swelling in the left lower Limb on the lateral aspect associated With itching, local rise of temperature and redness.Pigmentation is seen and swelling was associated with pain which is throbbing in nature non radiating type no aggrevating or releiving factors.
Dorsalis pedis artery is felt.
Erythematous rash is present on the cheek bilaterally.It is not associated with itching now. 10days back there was itching which gradually subsided.
SYSTEMIC EXAMINATION
CVS:-
INSPECTION: Shape of chest in normal
no visible neck veins
No rise in JVP
No visible pulsation scars.
PALPATION: All inspectory findings are confirmed.
Cardiac impulse felt at 5th intercostal space 1cm medial to the mid clavicular line.
PERCUSSION: shows normal heart borders
AUSCULTATION: S1 S2 heard no murmurs
CNS:-
Normal tone and power.
Sensory system : touch vibration proprioception normal.
MOTOR SYSTEM: Normal tone and power
REFLEXES: Right Left
BICEPS 2+ 2+
TRICEPS 2+ 2+
SUPINATOR 2+ 2+
KNEE 2+ 2+
CRANIAL NERVE EXAMINATION:-
2nd cranial nerve Right Left
Visual acuity Counting fingers positive
Direct light reflex present. Present
Indirect light reflex present. Present
Perception of light. Present. Present
Remaining cranial nerves normal.
GIT SYSTEM:-
INSPECTION: normal scaphoid abdomen with no pulsations and scars
PALPATION: inspectory findings are confirmed
no organomegaly, non tender and soft
PERCUSSION: normal resonant note present, liver border normal
AUSCULTATION: normal abdominal sounds heard, no bruit present
RESPIRATORY SYSTEM:
INSPECTION: Shape of chest is elliptical,
B/L symmetrical chest,
Trachea in central position,
Expansion of chest- left normal
Right - decreased
PALPATION: All inspectory findings are confirmed,
No tenderness, No local rise of temperature,
trachea is deviated to the right,
Tactile vocal fremitus: decreased on right side ISA, InfraSA, AA, IAA.
PERCUSSION: Dull note present in right side ISA, InfraSA, AA, IAA.
AUSCULTATION: B/L air entry present, vesicular breath sounds heard
Decreased intensity of breath sounds in right SSA,IAA
INVESTIGATIONS:-
ANA REPORT:

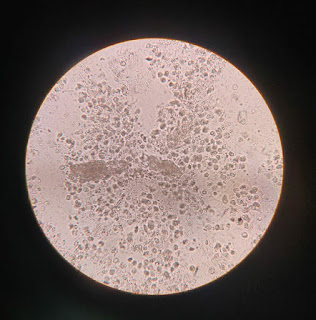
HEMATOLOGY:
IMPRESSION: Normocytic hypochromic ( Hb 6.0 )
Mild decrease in Platelet count
Relative monocytosis
CHEST X- RAY:
PROVISIONAL DIAGNOSIS:
SECONDARY SJOGRENS SYNDROME
LEFT LOWER LIMB CELLULITIS WITH BILATERAL OPTIC ATROPHY
TREATMENT:
1.INJ PIPTAZ 4.5 gm IV/ TID.
2.INJ METROGEL100 ML IV/TID
3.INJ NEOMOL1GM/IV/SOS
4.TAB CHYMORAL FORATE PO/TID
5.TAB PAN 40 MG PO/ OD.
6.TAB TECZINE10 MG PO/OD
7.TAB OROFERPO/OD.
8.TAB HIFENAC-P PO/OD
9HYDROCOTISONE cream 1%on face for 1week.
--------------------------------------------------------------------------
SHORT CASE
CASE PRESENTATION :
A 46 year old male came with chief complaints of:
Burning micturition present since 10 days
Vomiting since 2 days ( 3 - 4 episode)
Giddiness and deviation of mouth since 1 day
HISTORY OF PRESENTING ILLNESS:
Patient was apparently asymptomatic 10years back,
he complained of polyuria for which he was diagnosed
with Type 2 diabetes mellitus he was started on OHAs.
3years back OHAs were converted to insulin.
2 days back, he developed vomiting , containing food
particles and non bilious. He also complained of
deviation of mouth and giddiness 1 day
His GRBS was also recorded high , for which he was
given NPH 10 IU and HAI 10 IU
No history of fever/cough/cold
No history of previous UTIs
No history of chest pains/palpitations/syncopal attacks
PAST HISTORY:
10yrs back patient was diagnosed with Type 2 DM.
3 years back , he underwent cataract surgery.
1 year back, he had h/o small injury on leg which
gradually progressed to non healing ulcer extending
upto below knee eventually ended with below knee
amputation due to development of wet gangrene.
Not a k/c/o HTN/Epilepsy/TB/BA/Thyroid disorder/CAD/CVD
PERSONAL HISTORY:
Diet - Mixed
Appetite- normal
Sleep- Adequate
Bowel and bladder- Regular
Micturition- burning micturition present
Habits/Addiction:
Alcohol-
Not consuming alcohol since 1 yr.
Previously (1yr back) Consumption of
alcohol, about 90mlwhiskey almost daily.
Also 1month on&off consumption pattern was
previously present.
FAMILY HISTORY:
Not significant
GENERAL EXAMINATION:
Vitals @ Admission:
BP: 110/80 mmHg
HR: 98 bpm
RR: 18 cpm
TEMP: 101F
SpO2: 98% on RA
GRBS: 124 mg/dL
Pallor present
No Icterus/Cyanosis/Clubbing/Koilonychia/Lymphadenopathy/Edema
No dehydration
Systemic Examination:
CVS: S1S2 heard, No murmurs
RS: BAE+,NVBS
P/A: Soft, Non tender
CNS:
Reflexes: (Biceps/Triceps/Knee/Ankle/Plantar)Normal
Power: Normal(5/5) in both Upper and Lower limbs
Tone: Normal in both Upper and Lower limbs
No meningeal signs
Investigations:
URINE FOR KETONE BODIES
X RAY KUB
LFT
RFT
Ultrasound abdomen and pelvis:
BACTERIAL CULTURE REPORT:
Culture report: Klebsiella pneumoniae positive:
Sodium- 130
Chloride- 97
Hb- 6.4
TLC- 13,700
Platelet count- 50000
Urea - 146
Creatinine- 4.2
Uric acid- 9.1
X ray KUB
PROVISIONAL DIAGNOSIS:
Right emphysematous pyelonephiritis
and left acute pyelonephiritis and encephalopathy
secondary to sepsis.
H/o of Type 2 Diabetes mellitus since 10years
TREATMENT:
INJ. MEROPENEM 500mg IV BD
INJ. ZOFER 4mg IV TID
INJ. RANTAC 50mg IV OD
INJ. LASIX 40 mg IV BD
IV Fluids- NS,RL @ 100 mL/hr
SYP. MUCAINE GEL 10 mL PO TID
INJ.HAI SC TID ACC to GRBS
TAB.DOLO 650 mg SOS



.png)
.png)
.png)
















Comments
Post a Comment