1701006091 CASE PRESENTATION
LONG CASE
1- Breathlessness (since 20 days)
2-Cough( since 20 days)
3-Fever(since 4 days)
HOPI:
Patient was apparently asymptomatic 20 days back,then he developed
Breathlessness- NYHA - Grade -2 and 3 aggrevated on exertion and on exposure to cold,associated with wheeze no orthopnea and no PND. Relieved on rest.
Cough with expoctoration - mucoid,non foul smelling and non blood stained, increased during night, no postural variations were seen, relieved on taking medication.
fever,low grade evening rise of temperature,not associated with chills and rigors.
Loss of appetite and loss of Weight are seen.
Past History:
No H/O similar complaints in the past.
No H/O pulmonary tuberculosis and COVID -19.
No H/O diabetes, hypertension,CAD and epilepsy.
Personal History:
Appetite: decreased
Diet: mixed
sleep: adequate
Bowel and bladder: Regular
addictions:H/o BD Smoking since 50 years (4-5 BD's per day)
Family History:
Insignificant.
GENERAL EXAMINATION:
Patient is concious, coherent and oriented to time,place and person.
Vitals:
Pulse rate: 102 BPM
Respiratory rate: 26 CPM
BP: 110/80.
spO2: 96% at room air
SYSTEMIC EXAMINATION:
Respiratory Examination:
Inspection :
shape of the chest: Bilaterally symmetrical and elliptical.
chest movements: decreased on right side
no kyphosis and scoliosis
no scars( sinuse, visible pulsations and engorged veins)
no usage of accessory muscles.
muscle wasting- present
Palpation:
All inspectory findings are confirmed.
Trachea - shifted to right side.
No local rise of temperature.
chest movements- decreased on right side
spinoscapular distance- same on both sides.
chest expansion-
RT and Lt hemithorax
chest circumference- 31 cm
Transverse diameter- 27cm
anteroposterior diameter-20 cm
Percussion:
Right sided - ( impaired )
Auscultation:
Bronchial breath sounds are heard on right side
RT sided - ( decreased breath sounds)
Cvs examination:
S1 and S2 - present
Normal heart sounds
No cardiac murmurs.
Cns examination:
superficial reflexes - present
sensory and motor functions- normal
no focal neurological deficits
Per Abdomen:
bowel sounds- heard
soft, non tender,
no organomegaly
Investigations:
Right Upper lobe fibrosis with pleural effusion.
Treatment :
Inj- AUGMENTIN ( 2g i.v TID)
Inj- PAN -40 mg OD
Inj- Paracetamol- 650 mg BD
ASCORIL - CS ( 2 table spoons)
Nebulization with Budecort ( BD )
Duolen ( TID)
O2 inhalation ( 2-4 lit/ min to maintain SpO2> 94%
Tab - Azithromycin ( 500 mg- OD)
-------------------------------------------------------------------------------------
SHORT CASE
Abdominal Distension since 1 year
Facial puffiness since 1 year
Itching all over the body since 1 year
H/O PRESENT ILLNESS
PAST HISTORY
She is a denovo diabetic
Not a K/C/O /HTN/ asthma / Ischemic heart disease / epilepsy / TB
FAMILY HISTORY
NO SIGNIFICANT FAMILY HISTORY
PERSONAL HISTORY:
OCCUPATION -Daily wage worker , stopped going to work since 3 months
DIET MIXED
APPETITE -Decreased
SLEEP NORMAL
BOWEL AND BLADDER HABITS : decreased urine output
ADDICTIONS: No
Patient is concious coherent and coperative, well oriented to time palce and person.
VITALS
BP 110/80
PR 90bpm
TEMP 98.5degrees F
SPO2 98 @ RA
GRBS 106
No Pallor , ICTERUS , CYANOSIS, CLUBBING , LYMPHADENOPATHY ,
SYSTEMIC EXAMINATION
Inspection :
Abdomen is distended
Umbilicus is inverted
Movements :- gentle rise in abdominal wall in inspiration and fall during expiration.
No visible gastric peristalsis
palpation : SOFT, NON TENDER, NO ORGANOMEGALY
RS - BAE + , normal vesicular breath sounds

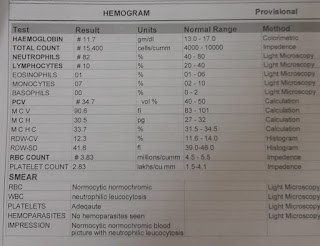
Renal function test
Liver function test
Complete blood picture
Lipid profile
Ultrasound:
X-ray
Provisional diagnosis : Steroid induced cushings syndrome with tenia corporis infection
Treatment:
4-06-2022
Inj. Pantop
Inj lasix
Inj optineuron
Tab. Ultracet
Tab . Zofer
Luliconazole
Syp aristozyme
5-06-2022
Ultracet
Luliconazole ointment
Rantac
Syp aristozyme
6-06-2022
Ultracet
Luliconazole ointment
Rantac
T defloz 6mg
Syp. Aristozyme
7-06-2022
Ultracet
Luliconazole ointment
Rantac
Syp. Aristozyme


















Comments
Post a Comment