1701006096 CASE PRESENTATION
LONG CASE
A 59 years old female who is a house maker , resident of Nalgonda has presented to the opd with the chief complaints of
- Generalised weakness since 6 months
- Facial puffiness since 6 months
- Decreased urinary output since 3 months
Time line of events
HISTORY OF PRESENT ILLNESS
Patient was apparently asymptomatic 1year back later she went to a local rmp for regular checkup and there she was diagnosed with hypertension and was on medication
6 months back patient complaint of decreased food intake , weakness , puffiness of face and legs so went to near by hospital. But there was no improvement
5 months back they went to Miralguda hospital with reduced food intake, weakness, puffiness of face, Patient complained of bilateral pedal edema of grade 2 below the knees which was insidious in onset, gradually progressive, pitting type, increased as the day progressed and had no relieving factors
They came to Kamineni Hospital in the month of April
Here the patient was put on dialysis which was
done weekly 2 times.
Patient usually wakes up at 5 am and will do household works and have breakfast along with coffee at 8am again continues her household work and then she will have her lunch which is rice, dal at 1:00pm and then takes a nap again continues her work then will have her dinner which is rice and dal at 8:30pm and goes for sleep at 10:00 pm.
PAST HISTORY
Known case of hypertension since 1yr
Not a known case of Diabetes mellitus , tuberculosis , asthma, epilepsy
No history of similar complaints in the past
No previous surgical history
PERSONAL HISTORY
Diet- Mixed
Appetite- Decreased since 1 month
Bowel and bladder movements- Urine frequency is reduced since 3 monthsBowel movements are regular
Sleep- Adequate
Addictions- no
No history of drug or food allergies
FAMILY HISTORY No similar complaints in the family
GENERAL EXAMINATION Done after obtaining consent, in the presence of attendant with adequate exposurePatient is conscious, coherent, cooperative and well oriented to time, place and personPatient is not well nourished and not moderately built Pallor present Pedal edema- present- bilateral pitting type
No history of cyanosis, clubbing and lymphadenopathy
VitalsTemperature- Afebrile
Blood pressure- 150/90 mm of Hg
Pulse rate- 86 bpm
Respiratory rate- 21cpm
SpO2 : 98% At room air
SYSTEMIC EXAMINATION
Abdomen examination
On Inspection:
-Shape of the abdomen- Distended
-Umbilicus- inverted
-Movements of abdominal wall- moves with respiration
-Skin is smooth
-No visible peristalsis, pulsations, sinuses, engorged veins, hernial sites
On Palpation :
-Inspectory findings are confirmed
-Soft and non tender
-No palpable mass
-Liver and spleen not palpable
On Percussion:
-Dullness is noted
On Auscultation:
-Bowel sounds heard
Cardiovascular system examination:S1 and S2 sounds are heardNo murmurs
Respiratory system examination:Bilateral air entry presentNormal vesicular breath sounds are heard
Central nervous system examination:No focal neurological deficits
Clinical pictures:
HISTORY :
A 50 year old male patient who is a farmer and a daily wage worker by occupation, a resident of Pochampally, came to the opd with
CHIEF COMPLAINTS :
There is no local rise of temperature.
No hepatomegaly. No splenomegaly.
Guarding is present.
Rigidity is absent.
Kidney not palpable.
Shifting dullness : Positive
Liver span could not detected
Auscultation :
Bowel sounds are decreased.
Cardiovascular System : S1, S2 heard
Respiratory System : Normal vesicular breath sounds heard
Central Nervous System : Conscious; Speech normal ; Motor and sensory system examination is normal, Gait is normal.
INVESTIGATIONS :
1. Hemogram :
Hemoglobin : 9.8g/dl
TLC : 7,200
Neutrophils : 49%
Lymphocytes : 40%
Eosinophils : 1%
Basophils : 0%
PCV : 27.4%
MCV : 92.3 fl
MCH : 33 pg
MCHC : 35.8%
RDW-CV : 17.6%
RDW-SD : 57.8 fl
RBC count : 2.97 millions/mm3
Platelet count : 1.5 lakhs/mm3
Smear : Normocytic normochromic anemia
2. Serology :
HbsAg : Negative
HIV : Negative
3. ESR :
15mm/1st hour
4. Prothrombin time : 16 sec
5. APTT : 32 sec
6. Serum electrolytes :
Sodium : 133 mEq/L
Potassium : 3 mEq/L
Chloride : 94 mEq/L
7. Blood Urea : 12 mg/dl
8. Serum Creatinine : 0.8 mg/dl
9. LFTs :
Total Bilirubin : 2.22 mg/dl
Direct Bilirubin : 1.13 mg/dl
AST : 147 IU/L
ALT : 48 IU/L
ALP : 204 IU/L
Total proteins : 6.3 g/dl
Serum albumin : 3 g/dl
A/G ratio : 0.9
10. Ascitic fluid :
Protein : 0.6 g/dl
Albumin : 0.34 g/dl
Sugar : 95 mg/dl
LDH : 29.3 IU/L
SAAG : 2.66 g/dl
11. Ascitic Fluid Cytology :
12. Ascitic fluid culture and sensitivity report :
13. Ultrasound :
Coarse echotexture and irregular surface of liver - Chronic liver disease
Gross ascites
Gallbladder sludge
14. ECG
15. X-ray
PROVISIONAL DIAGNOSIS :
Decompensated Chronic liver disease with ascites most likely etiology is alcohol.
TREATMENT :
Drugs :
1. Inj. Pantoprazole 40 mg IV OD
2. Inj. Lasix 40 my IV BD
3. Inj. Thiamine 1 Amp in 100 ml IV TID
4. Tab. Spironolactone 50 mg BB
5. Syrup Lactulose 15 ml HS
6. Syrup Potchlor 10ml PO TID
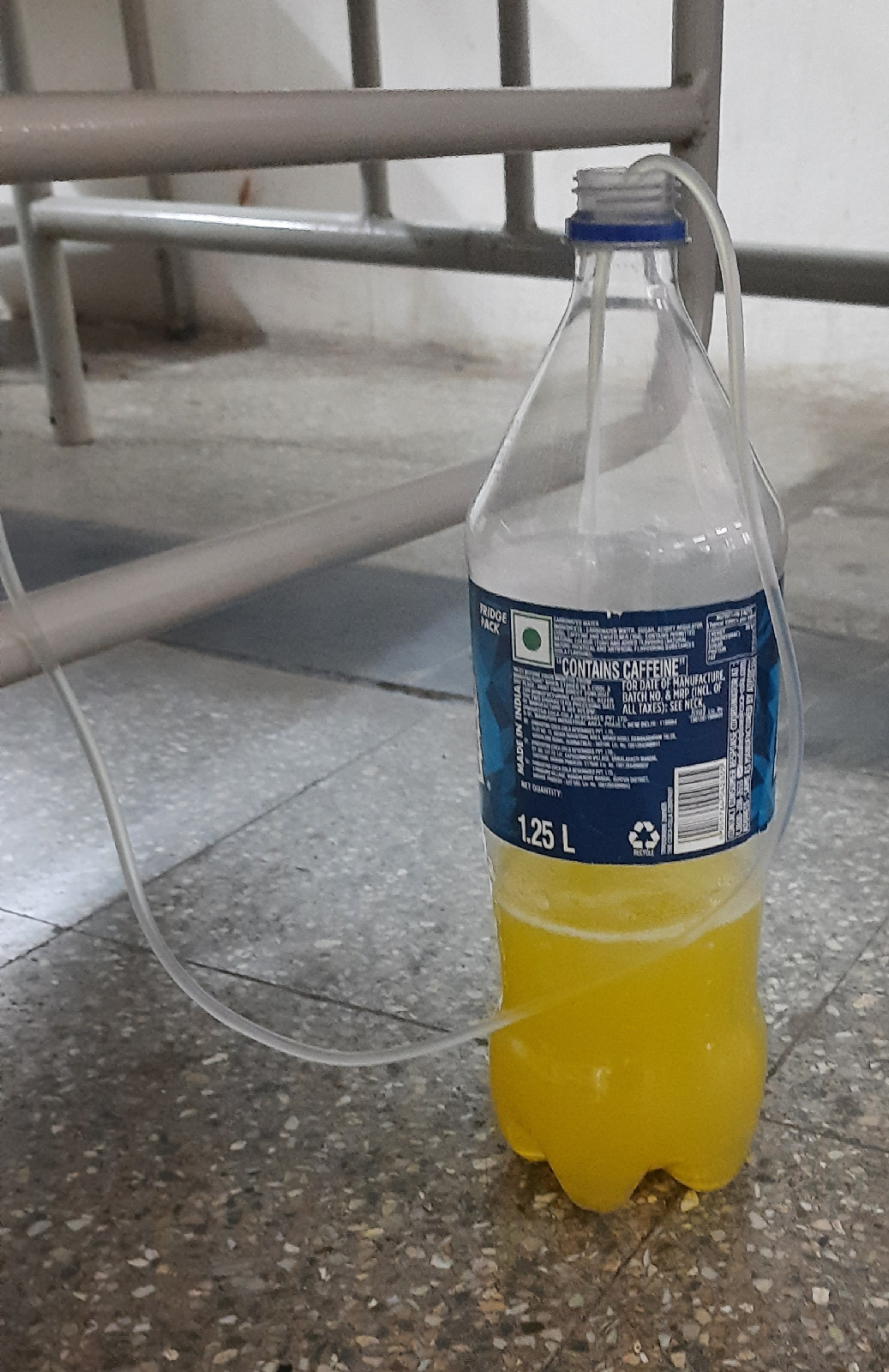
7. Fluid restriction less than 1L/day
8. Salt restriction less than 2g/day
Ascitic fluid tapping :
Ascitic fluid was tapped)






































Comments
Post a Comment