LONG CASE
A 65 year old male toddy climber by occupation came to the casualty with cheif complaints of
- fever since 3days
-abdominal distention since 2days
-urinary retention since 2days
History of presenting illness:
-Patient was apparently asymptomatic 3days back later he developed fever which was on and off, low grade type of fever, without any diurnal variation and relieved on taking medication,
-later he developed abdominal distension which was insidious in onset, gradually progressive to the current size, no aggrevating and relieving factors.
-He also complained of urinary retention since 2days associated with burning micturition .
- No history of chills, rigors vomiting, nausea, loose stools and pain in the abdomen.
Past history:
10 years back he had swelling and pain abdomen ;was diagnosed with left sided inginal hernia, operated , preoperative and post operative period uneventful.
4 years back patient had complaint of giddiness ; was diagnosed with Hypertension ,on medication.
6months back patient had complaint of bipedal edema ; investigations were done ct scan showed unilateral (left) stag horn renal calliculi.
1 month back he developed fever , on and off low grade type, tightness in abdomen, facial puffiness, shortness of breath, decreased appetite, pedal edema for which he was investigated and treated conservatively. (file)
(file) (present)
(present)
Personal history:
appetite: decreased,
Diet: mixed,
Sleep: adequate,
Bowel and blader habits: regular,
Burning micturition present,
Addictions: alcohol consumption occasionally, (one quarter a month) stopped 6 months ago.
Family history:
No significant familial history.
General examination:
Patient was conscious, coherent, cooperative. Oriented to time place and person.
Moderately built and moderately nourished.
No signs of pallor, icterus, cyanosis, clubbing, koilynchia, lymphadenopathy.
Edema - present , pitting type , grade 1
Vitals:
Temperature: 98.7°F
Pulse rate: 82bpm
Respiratory rate: 17cpm
Blood pressure: 140/70mmhg
Spo2: at room air 99%
GRBS: 134mg%
Local examination:
Abdomen
Patient was examined in supine position in a well lit room , with consent taken .
Inspection:
Shape of abdomen: distended
Umbilicus: everted
Movements of abdominal wall ,moves with respiration.
Scar of previous herina surgery seen at inginal region.
No visible pulsations , venous engorgement, sinuses.
Skin appears to be normal.
Palpation:
No local raise of temperature,
Tenderness -mild tenderness in suprapubic region and right hypochondrium.
Tense abdomen,
Bimanual palpation of kidney: non ballotable.
No organomegaly.
Percussion:
Normal resonant notes present over the abdomen
Liver dullness at fifth intercostal space.
Auscultation:
Normal bowel sounds were heard, no bruit present
Systemic examination:
Cvs: S1,S2 heard , apex beat- normal, no murmurs.
Respiratory system: Bilateral air entry present, normal vescular breath sound heard.
CNS: no sensory or motor abnormalities seen, cranial nerves:normal, higher mental functions: normal, No meningeal signs , No cerebral signs.
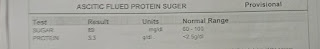
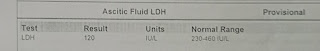
Investigations:
Provisional diagnosis:
CKD on MHD, with multiple renal calliculi in left kidney,With grade 4 renal pelvic dilatation.
Also a known case of hypertension since 4years.
Management:
Injection. Piptaz 2.25grs,iv,/bd
Injection. Metronidizole 0.5%gm/100ml
Tab.lasix 40mg/bd
Tab.nodosis 500mg/bd
Tab.pan 40mg/od
Tab.orofer XT /od
Tab. Shelcal 500mg/od
Tab.nicardia 20mg/bd
Syrup. aristozyme 15ml/bd.
------------------------------------------------------
SHORT CASE
A 28year old female presented to casualty with complaints of
-headache since 3 days,
-Fever since 3 days,
-Decreased appetite since 3 days .
History of presenting illness:
Patient was apparently asymptomatic 8 days back later she ingested rodenticide (zinc phosphide) of aprroximatly:12-14grms
After ingestion ; two episodes of vomiting, abdominal pain , difficulty in speech and altered behaviour. Was treated for the same.
3 days back she developed generalized headache, no aggrevating and reliving factors, fever continuous low grade type ,not associated with chills and rigors. Associated with decreased appetite.
No history of loss of consciousness, seizures, sob , involuntary defecation and micturition.
No history of Loose stools.
Past history:
No similar complaints in the past.
Not a know case of DM, HTN, TB, asthama, or any other chronic illness.
Personal history:
Appetite: decreased
Diet :mixed
Bowel and bladder : regular
Sleep : adequate.
No addictions.
General examination:
patient was conscious, coherent, cooperative, oriented to time, place and person.
No pallor, icterus ,cyanosis ,clubbing, koilynchia lymphadenopathy ,edema.
Vitals:
Temperature:100°F
Pulse rate: 100bpm
Respiratory rate: 15cpm
Blood pressure: 110/80mmhg
Spo2 at room air: 97%
GRBS: 133mg%
Systemic examination:
CNS:
Level of consciousness: drowsy but arousable
Speech: aphasic
No meningeal signs
Glassgowcoma scale: E4,V1,M6. (11/15).
CVS: S1 S2 heard, apex beat-normal, no murmurs and bruits.
Respiratory system: bilateral air entry present, normal vescular breath sounds heard.
Per abdomen: soft, nontender, no organomegaly.
Investigations:
Deranged pt , aptt .
Provisional diagnosis:
Zinc phosphide poisioning. (Rodenticide)
Management:
Regular monitoring of vitals
Treatment:1.INJ NAC 50MG/KG IN 500ML DNS
2.INJ PANTAPRAZOLE 40MG IV/OD
3.INJ ONDENSETRON 4MG Iv/OD
4.INJ NAC 1GM IV/OD
5.INJ VIT K 10MG IM STAT
6.CAP EVION 400MG PO OD
7. INJ SODIUM BICARBONATE 50MEQ /IV/STAT
8. INJ.SODA BICARB 1MEQ/KG/HR/IV
9. INJ.FUROSEMIDE 20MG/IV/BD
10. SYP SUCRALFATE 10ML POTID
11 .OPTINEURON 1 AMPOULE IN 500ML NS
















Comments
Post a Comment