1701006102 CASE PRESENTATION
LONG CASE
A 35 year old male, bartender by occupation, resident of Sathupalli, Khammam district, came to the hospital with the following chief complaints --
- shortness of breath - from 10 days
- cough- from 2 days
- palpitations - from 7 days
- Pedal edema from 2days.
- 1 month ago, he developed shortness of breath while lying down, then he visited local RMP, where he was given an injection? and symptoms subside for a while. He experienced symptoms after consumption of alcohol.
- later he visited another doctor, few investigations were done and was told to have a heart problem?
- insidious onset
- mucopurulent
- sudden in onset
- no associated with chest pain
- NO history of similar complaints in the past.
- Not a known case of Diabetes, Hypertension, Tuberculosis, Asthma, hypothyroidism/hyperthyroidism, COPD, and blood transfusions.
- no history of previous surgeries'
- Diet: mixed
- Appetite: reduced from past 10 days
- Bowel habits: normal
- Bladder habits: normal
- Sleep: disturbed from past 10 day
- Addictions:
- Built and nourishment: moderately built and moderately nourished
- Pallor: No pallor
- Icterus: No icterus
- Cyanosis: No cyanosis
- Clubbing: No clubbing
- Generalized lymphadenopathy: No generalized lymphadenopathy
- Pedal edema: No pedal edema
- Temperature afebrile
- Pulse 140-160 bpm (irregularly irregular)
- Respiratory rate : 30 per minute
- Bp 130/90
- Spo2 98%
- GRBS 132 mg%
- The chest wall is bilaterally symmetrical
- No dilated veins, scars or sinuses are seen
- Apical impulse or pulsations cannot be appreciated
- Apex beat is shifted to 6th inter coastal space , 2-3cm deviated from mid clavicular line
- No parasternal heave felt
- No thrill felt
- Right and left borders of the heart are percussed
- S1 and S2 heard
- Shape- elliptical
- B/L symmetrical ,
- Both sides moving equally with respiration .
- Trachea - central
- Expansion of chest is symmetrical.
- Vocal fremitus - normal
- resonant bilaterally
- bilateral air entry present.
- wheeze is present in all areas
- Shape – elliptical
- Flanks – full
- Umbilicus –everted
- All quadrants of abdomen are moving with respiration.
- No dilated veins, hernial orifices, sinuses
- No visible pulsations.
- Apical Impulse is not appreciated
- Chest is moving normally with respiration.
- No dilated veins, scars, sinuses.
Palpation :
- No local rise of temperature and tenderness
- All inspectory findings are confirmed.
- No guarding, rigidity
Percussion:
- There is no fluid thrill , shifting dullness.
- Percussion of liver for liver span
- Percussion of spleen- dull note
Auscultation:
- Bowel sounds are feeble.
4.CENTRAL NERVOUS SYSTEM EXAMINATION:
HIGHER MENTAL FUNCTIONS:
Patient is Conscious, well oriented to time, place and person.
All cranial nerves - intact
Motor system
Right. Left
BULK
Upper limbs. N N
Lower limbs N N
TONE
Upper limbs. N. N
Lower limbs. N N
POWER
Upper limbs. 5/5. 5/5
Lower limbs 5/5. 5/5
Superficial reflexes and deep reflexes are present , normal
Gait is normal
No involuntary movements
Sensory system - all sensations ( pain, touch, temperature, position, vibration sense) are well appreciated .
- serum creatinine : 1.0 mg\dl
- blood urea : 22mg\dl
- serum electrolytes : Na+ - 138 mEq\L
- K+ - 3.9
- Cl- - 100
- Ph : 7.43
- PCo2 : 26.8 mmHg
- PO2 : 76.3 mmHg
- HCo3: 17.6 mmol\L
- St. HCo3 : 20.4 mmol\L
- TCo2 : 35
- O2 stat : 94.0
- hemoglobin : 12.0 gm\dl
- TLC : 14,000
- PCV : 37.6
- MCV : 70.9
- MCH : 22.4
- RDW-CV : 16.9
- total bilirubin : 2.32
- direct bilirubin : 0.64
- SGPT : 58
- SGOT : 34
- Ph : 7.43
- PCo2 : 26.8 mmHg
- PO2 : 76.3 mmHg
- HCo3: 17.6 mmol\L
- St. HCo3 : 20.4 mmol\L
- TCo2 : 35
- O2 stat : 94.0
- Hb : 11.3
- TLC : 17,100
- platelets : 3.43
- inj AMIODARONE 900mg in 32 ml normal saline @ 0.5mg\min
- inj AUGMENTIN 1.2gm\IV\BD
- tab AZITHROMYCIN 500mg PO\BD
- inj HYDRODRT 100mg IV\BD
- neb with DUOLIN @ 8th hourly
- inj LASIX 40mg\IV\BD
- inj THIAMINE 200mg in 50ml normal saline IV\TID
- tab CARDARONE 150mg
- tab clopitab 75mg RO OD
- tab ATROVAS 80MG
- Fluid restriction <1.5L per day
- Salt restriction <4gm per day
- Strict temperature chart 4th hourly
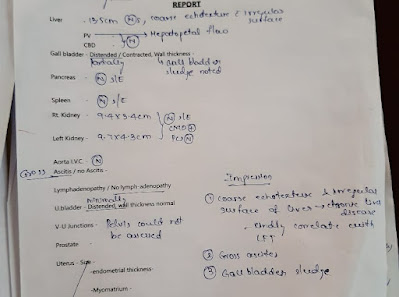
50 year old male, farmer by occupation, resident of Yadadri, came to the hospital with the following chief complaints --
- Distended abdomen - from 7 days
- Pain abdomen- from 7 days
- Pedal edema- from 5 days
- Breathlessness- from 4 days
- insidious in onset,
- gradually progressive,
- aggravated in last 4 days and progressed to the present
- insidious in onset,
- gradually progressive,
- colicky type in the epigastrium and right hypochondrium
- Grade II since 3 days
- insidious in onset,
- Gradually progressive,
- pitting type
- bilateral
- below knees
He also complained of shortness of breath since 4 days - MRC grade 4
- Insidious in onset
- Gradually progressive
- Aggravated on eating and lying down
Patient is a known alcoholic since 20 years, he stopped 6 months back. Ascites increased after his last drink on 29th May, 2022.(beer and toddy)
- NO history of similar complaints in the past.
- Not a known case of Diabetes, Hypertension, Tuberculosis, Asthma, hypothyroidism/hyperthyroidism, COPD, and blood transfusions.
- no history of previous surgeries'
- Diet: mixed
- Appetite: reduced
- Bowel habits: frequency of urine is reduced since 2 days
- Bladder habits: constipation since last 4 days
- Sleep: disturbed
- Addictions:
- Beedi smoker: for past 30 years. 4-5 beedis per day
Alcohol
- Whiskey-90 ml, 2 times a week, since 5 years
- Built and nourishment: moderately built and moderately nourished
- Pallor: No pallor
- Icterus: No icterus
- Cyanosis: No cyanosis
- Clubbing: No clubbing
- Generalized lymphadenopathy: No generalized lymphadenopathy
- Pedal edema: Grade II bilateral pedal edema

- Shape of the abdomen: globular
- Distension of abdomen: distended
- Flanks: full
- Umbilicus:
- Shape: everted
- Position: central
- Movements of abdominal wall - moves with respiration
- Skin is smooth and shiny
- No scars, sinuses, distended veins, striae.
- Local rise of temperature present.
- Tenderness present - epigastrium.
- Tense abdomen
- Guarding present
- Rigidity absent
Fluid thrill positive
- Liver not palpable
- Spleen not palpable
- Kidneys not palpable
- Lymph nodes not palpable
PERCUSSION:
- Liver span : not detectable
- Fluid thrill: felt
AUSCULTATION:
- Bowel sounds: heard in the right iliac region
- The chest wall is bilaterally symmetrical
- No dilated veins, scars or sinuses are seen
- Apical impulse or pulsations cannot be appreciated
- Apical impulse is felt in the fifth intercostal space
- No parasternal heave felt
- No thrill felt
- Right and left borders of the heart are percussed
- S1 and S2 heard
- Shape- elliptical
- B/L symmetrical ,
- Both sides moving equally with respiration .
- Trachea - central
- Expansion of chest is symmetrical.
- Vocal fremitus - normal
- resonant bilaterally
- bilateral air entry present.
- Normal vesicular breath sounds heard.
CNS EXAMINATION:
- Conscious
- Speech normal
- Cranial nerves: normal
- Sensory system: normal
- Motor system: normal
Reflexes: Right. Left.
Biceps. ++. ++
Triceps. ++. ++
Supinator ++. ++
Knee. ++. ++
Ankle ++. ++
Gait: normal
Hemogram :
Hemoglobin : 9.8 g/dl
TLC : 7,200
Neutrophils : 49%
Lymphocytes : 40%
Eosinophils : 1%
Basophils : 0%
PCV : 27.4%
MCV : 92.3 fl
MCH : 33 pg
MCHC : 35.8%
RDW-CV : 17.6%
RDW-SD : 57.8 fl
RBC count : 2.97 millions/mm3
Platelet count : 1.5 lakhs/mm3
Smear : Normocytic normochromic anemia
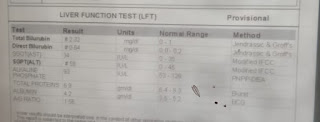
Liver function tests:
Total Bilirubin : 2.22 mg/dl
Direct Bilirubin : 1.13 mg/dl
AST : 147 IU/L
ALT : 48 IU/L
ALP : 204 IU/L
Total proteins : 6.3 g/dl
Serum albumin : 3 g/dl
A/G ratio : 0.9
- ESR :
15mm/1st hour
- Prothrombin time : 16 sec
- APTT : 32 sec
- Serum electrolytes :
Sodium : 133 mEq/L
Potassium : 3 mEq/L
Chloride : 94 mEq/L
- Blood Urea : 12 mg/dl
- Serum Creatinine : 0.8 mg/dl
- Ascitic fluid :
Protein : 0.6 g/dl
Albumin : 0.34 g/dl
Sugar : 95 mg/dl
LDH : 29.3 IU/L
SAAG : 2.66 g/dl
- Serology :
HbsAg : Negative
HCV : Negative
HIV : Negative















































Comments
Post a Comment