LONG CASE
50 year old male patient with weakness of the lower limbs bilaterally since 2 days.
He is a resident of Nalgonda, and a daily wage worker till one year ago. He had a fainting episode after which he stopped going to work.
HISTORY OF PRESENT ILLNESS:
Patient was apparently asymptomatic 4 months back , when he developed pain in the right hip region, which was insidious in onset and intermittent at the beginning.
Pain aggravated on movement and relieved on rest and medication.
He went to the hospital 2 months ago when the pain progressed and became continuous and was diagnosed with avascular necrosis of the femur due to a trauma to the hip one year ago.
2 days ago, patient developed weakness in the lower limb which progressed upto the hip.
The next morning, patient required assistance to walk and sit up but was able to feed himself.
The weakness progressed and by evening he was unable to feed himself. He only responded if called to repeatedly.
The weakness was not associated with loss of consciousness, slurring of speech, drooping of mouth, seizures, tongue bite or frothing of mouth, difficulty in swallowing.
No complaints of any headache, vomitings, chest pain, palpitations and syncopal attacks.
No shortness of breath, orthopnea, paroxysmal nocturnal dyspnea, abdominal pain or burning micturition.
HISTORY OF PAST ILLNESS:
No similar episodes in the past.
Patient is a known case of diabetes since 12 years. He is on regular medication, with 15 U INSULIN in the morning before breakfast and 10 U in the evening (7-7:30pm).
He was hospitalized, 4 years ago with low blood sugar, and was admitted for 10 days. He presented with altered mental status.
No history of hypertension, tuberculosis, epilepsy, asthma, thyroid and CAD.
No surgical history.
PERSONAL HISTORY:
Diet: Mixed
Appetite: Normal
Sleep: Adequate
Bowel and Bladder: Regular bladder, decreased bowel movements.
No allergies
Started alcohol intake 25 years back, stopped 12 years when diagnosed with diabetes. He used to binge drink alcohol for 10 days continuously every month and then used to stop for 20 days. Cycle repeats every month. Now, consuming alcohol only on special occasions, doesn't exceed 90ml.
Started smoking beedis, one a day, 10 years ago.
Stopped 4 years ago when he went into a hypoglycemic episode, but has resumed one year ago.
FAMILY HISTORY:
No similar complaints in family.
GENERAL EXAMINATION:
Patient is examined in a well lit room after taking informed consent.
Patient is conscious, coherent and cooperative.
He is moderately built and moderately nourished.
Pallor: Present
Icterus: absent
Cyanosis: absent
Clubbing: absent
Generalized Lymphadenopathy: absent
Edema: Absent
VITALS:
Temperature: Afebrile
Blood Pressure: 124/72 mmHg
Respiratory Rate: 17 cycles per minute
Pulse: 70 bpm
SYSTEMIC EXAMINATION:
CENTRAL NERVOUS SYSTEM EXAMINATION.
Higher mental functions
• conscious
• oriented to person and place
• memory - able to recognize their family members and recall recent events
• Speech - no deficit
Cranial nerve examination
• 1 - couldn't be elicited
• 2- Direct and indirect light reflex present
• 3,4,6 - no ptosis Or nystagmus
• 5- corneal reflex present
• 7- no deviation of mouth, no loss of nasolabial folds, forehead wrinkling present
• 8- able to hear
• 9,10- position of uvula is central
• 11- sternocleidomastoid contraction present
• 12- no tongue deviation
Motor system
Attitude - right lower limb flexed at knee joint
Right Left
BULK
Arm. 22 cm. 22cm
Forearm. 20.5cm 20.5cm
Thigh. 34cm. 34cm
Leg. 26cm. 26cm
TONE
Upper limbs. N. N
Lower limbs. N N
POWER
Upper limb
Elbow- Flexor. 5/5. 5/5
Extensor 5/5 5/5
Wrist- Flexor. 5/5. 5/5
Extensor 5/5. 5/5
Hand grip. 5/5. 5/5
Lower limb
Hip- Flexors. 5/5. 5/5
Extensors. 5/5. 5/5
Knee- Flexors. 5/5. 5/5
Extensors. 5/5. 5/5
Ankle- DF. 5/5. 5/5
PF. 5/5. 5/5
EHL. 5/5. 5/5
FHL. 5/5. 5/5
REFLEXES. Right. Left
Biceps. 2+ 2+
Triceps. 2+ 2+
Supinator. 2+ 2+
Knee. 2+ 2+
Ankle. 2+ 2+
Gait is normal
No involuntary movements
Sensory system - all sensations ( pain, touch, temperature, position, vibration sense) are normal.
CARDIOVASCULAR SYSTEM
Chest wall - bilaterally symmetrical
No dilated veins, scars, sinuses
Apical impulse and pulsations cannot be appreciated
PALPATION:
Apical impulse is felt on the left 5th intercoastal space 2cm away from the midline.
No parasternal heave, thrills felt.
PERCUSSION:
Right and left heart borders percussed.
AUSCULTATION:
S1 and S2 heard , no added thrills and murmurs heard.
RESPIRATORY SYSTEM
INSPECTION:
Chest is bilaterally symmetrical
Trachea – midline in position.
Apical Impulse is not appreciated
Chest is moving normally with respiration.
No dilated veins, scars, sinuses.
PALPATION:
Trachea – midline in position.
Apical impulse is felt on the left 5th intercoastal space.
Chest is moving equally on respiration on both sides?
PERCUSSION:
The following areas were percussed on either sides-
Supraclavicular
Infraclavicular
Mammary
Axillary
Infraaxillary
Suprascapular
Infrascapular
Upper/mid/lower interscapular were all RESONANT.
AUSCULTATION:
Normal vesicular breath sounds heard
No adventitious sounds heard.
ABDOMEN EXAMINATION
INSPECTION:
Shape – scaphoid
Flanks – free
Umbilicus –central in position , inverted.
All quadrants of abdomen are moving equally with respiration.
No dilated veins, hernial orifices, sinuses
No visible pulsations.
PALPATION:
No local rise of temperature and tenderness
All inspectory findings are confirmed.
No guarding, rigidity
Deep palpation- no organomegaly.
PERCUSSION:
There is no fluid thrill , shifting dullness.
Percussion over abdomen- tympanic note heard.
AUSCULTATION:
Bowel sounds are heard.
BILATERAL LOWER LIMB WEAKNESS DUE TO AN ENDOCRINAL OR METABOLIC CAUSE IN A PATIENT WITH DIABETES MELLITUS WITH A HISTORY OF AVASCULAR NECROSIS OF HEAD OF FEMUR.
INVESTIGATIONS:
HEMOGRAM:
Hemoglobin: 8.6
TLC: 18380
N/L/E/M: 86/06/1/5
Platelet: 2.02
MCV: 71.6
MCH: 24.2
RDW: 15
PCV: 26.4
RBC COUNT: 3.63
ELECTROLYTES:
Na: 145
Cl: 110
K: 2.5
RENAL FUNCTION TESTS
Urea: 74
Creatinine: 3.7
Urine protein / creatinine: 0.27
Spot urine protein: 14.2 mg/ dl
Spot urine creatinine: 51.1mg/dl
LIVER FUNCTION TESTS
Total Bilirubin: 1.34
Direct Bilirubin: 0.55
SGOT:24
ALT:12
ALP:259
Total Protein: 6.3
Albumin: 2
A/G: 0.73
GRBS
On day 1
4:30 pm - 272gm/dl
On day 2
8am - 178/dl ( 4U HAI)
12pm- 205mg/dl
8pm - 176 mg/dl ( 8U HAI)
On day 3
12am - 120mg/dl
8am - 180mg/dl
2pm - 223mg/dl ( HAI 12 U)
On day 4
12 am - 210mg/dl
8 am - 302mg/dl
8pm- 203mg/dl
On day 5
2 am - 75mg/dl
8 am - 160mg/dl
8pm 478mg/dl
10pm- 325 mg/dl
On 2/6
On 4/6
PROVISIONAL DIAGNOSIS:
TREATMENT:
on day 1
1) tab ecospirin 70mg OD
2) tab atorvas 10mg OD
3) inj NS, RL at 70ml/hr
4) syrup potchlor 15ml/po/tid
5) normal oral diet
6) inj HAI - TID
7) 2 amp KCL in 500ml NS slowly over 4-5 hrs
On day 2
1) tab ecospirin 70mg OD
2) tab atorvas 10mg OD
3) inj NS, RL at 70ml/hr
4) syrup potchlor 15ml/po/tid
5) normal oral diet
6) inj HAI - TID
7) proteolytic enema
8) syrup cremaffine
9) tab spironolactone
On day 3
1) tab ecospirin 70mg OD
2) tab atorvas 10mg OD
3) inj NS, RL at 70ml/hr
4) syrup potchlor 15ml/po/tid
5) normal oral diet
6) inj HAI - TID
7) proteolytic enema
8) syrup cremaffine plus 15ml/po/od
9) tab spironolactone 25mg/po/od
10) tab azithromycin 500mg OD
11) high protein diet
On day 4
1) tab ecospirin 70mg OD
2) tab atorvas 10mg OD
3) inj NS, RL at 70ml/hr
4) syrup potchlor 15ml/po/tid
5) normal oral diet
6) inj HAI - TID
7) tab ultracet QID
8) syrup cremaffine plus 15ml/po/od
9) tab spironolactone 25mg/po/od
10) tab azithromycin 500mg OD
11) high protein diet
On day 5
1) tab ecospirin 70mg OD
2) tab atorvas 10mg OD
3) inj NS, RL at 70ml/hr
4) syrup potchlor 15ml/po/tid
5) normal oral diet
6) inj HAI - TID
7) tab ultracet 1/2 po/ QID
8) syrup cremaffine plus 15ml/po/od
9) tab spironolactone 25mg/po/od
11) high protein diet









--------------------------------------------------------------------------
SHORT CASE
A 46 year old male came to casuality with chief complaints of
-burning micturition since 10days
-hiccups since 3days
-vomiting since 2days (3-4 episodes)
-giddiness and deviation of mouth since 1day.
HISTORY OF PRESENT ILLNESS:
Patient was apparently asymptomatic 10days back, when he developed burning micturition , not associated with fever and decreased urine output.
3 days back then pateint complaints of hiccups.
2 days back, patient developed vomitings , 4-5 episodes, containing food particles, non bilious.
Patient complaints of deviation of mouth and giddiness one day, he was brought to the hospital and his GRBS was recorded to be high for which he was given NPH 10 IU and HAI 10 IU.
No c/o fever/cough/cold/ abdominal pain.
No c/o chest pains/palpitations/syncopal attacks.
HISTORY OF PAST ILLNESS:
10years back patient complained of polyuria after which he was diagnosed with Type 2 Diabetes Mellitus, he was started on oral hypoglycemic agents(OHA), which he took on and off due to financial crisis.
3years back OHAs were replaced by Insulin, he is taking insulin three times a day before food regularly.
3years ago he underwent a cataract surgery in the right eye.
1year ago he had injury to his right leg, which gradually progressed to non healing ulcer extending upto below knee and ended with undergoing below knee amputation due to developement of wet gangrene.
Delayed wound healing was present- it took 2months to heal
Not a k/c/o Hypertension, Epilepsy,Tuberculosis, Thyroid
Not on any medication
No history of blood transfusion
PERSONAL HISTORY:
Diet : Mixed
Appetite : normal
Sleep : Adequate
Bowel and bladder : Regular bowel
Micturition : burning micturition present
Habits/Addiction:
Alcohol-
Not consuming alcohol since 1 yr.Previously (1yr back) Regular consumption of alcohol, about 90mL whiskey consumed almost daily.
FAMILY HISTORY:
Not significant
GENERAL EXAMINATION:
Patient is examined in a well lit room after taking informed consent.
He is moderately built and moderately nourished.
Pallor: Present
Icterus: absent
Cyanosis: absent
Clubbing: absent
Generalized Lymphadenopathy: absent
Edema: Absent
VITALS:
Temperature: 101F
Blood Pressure: 110/80mmHg
Respiratory Rate: 18 cycles per minute
Pulse: 98 bpm
SPO2: 98% on RA
GRBS: 124mg/dl
SYSTEMIC EXAMINATION:
ABDOMEN EXAMINATION
INSPECTION:
Shape – scaphoid
Flanks – free
Umbilicus –central , inverted.
All quadrants of abdomen are moving with respiration.
No dilated engorged veins
No visible pulsations, visible peristalsis and scars.
PALPATION:
No local rise of temperature and tenderness
All inspectory findings are confirmed.
No guarding, rigidity
Deep palpation-
Liver : palpable just below costal margin ( right)
Sleep : not palpable
Kidney : not palpable
PERCUSSION:
There is no free fluid
Percussion over abdomen- tympanic note heard.
AUSCULTATION:
Bowel sounds heard.
CVS: S1S2 heard, No murmurs
RS: BAE+,NVBS
CNS:
Higher function test:
Patient is having altered sensorium
Slurred speech
Not Orientated to time place person.
Memory couldn't be elicited as patient is in altered sensorium
Cranial nerves : intact
Motor system :
1. Bulk : right. Left
Upperlimb normal. Normal
Lowerlimb. thigh -N. Normal
Below knee amputated on R side
2. Tone :
Upperlimb. Normal. Normal
Lowerlimb. Normal. Normal
3. Power :
Neck: Normal
Trunk: Normal
Upper limb 5 5
Lower limb 5 5
4. Reflexes
Right Left
Biceps 2+. 2+
Triceps 2+ 2+
Supinator 2+ 2+
Knee - 2+
Ankle - 2+
Planter reflex Amputated flexion
Sensory system : normal
Meningeal signs : negative
PROVISIONAL DIAGNOSIS:
Right (emphysematous?) pyelonephiritis and left acute pyelonephiritis and encephalopathy secondary to sepsis.
H/o of Type 2 Diabetes mellitus since 10years.
INVESTIGATIONS:
ON DAY OF ADMISSION:
HEMOGRAM:
Hemoglobin: 8.0 g/dl
TLC: 22900 cells/cumm
N/L/E/M: 89/03/1/7
Platelet: 1.50
MCV: 73.5
MCH: 27.2
RDW: 11.7%
PCV: 21.6
RBC COUNT: 2.94
# NEUTROPHILIC LEUKOCYTOSIS.
ELECTROLYTES:
Na: 124
Cl: 80
K: 2.6
RENAL FUNCTION TESTS
Urea: 129
Creatinine: 4.7
Urine for ketone bodies- negative
Total Bilirubin: 1.52
Direct Bilirubin: 0.50
SGOT:21
ALT:10
ALP:275
Total Protein: 5.6
Albumin: 2.3
A/G: 0.72
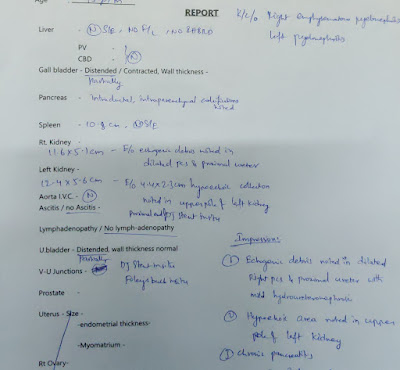
X-ray KUB
CT SCAN
ON DAY 2:
LDH- 192
24hr Urinary protein- 434
24hrs Urinary creatinine- 0.5
ON DAY 3
Hemoglobin- 6.8g%
TLC- 22,500cells/cumm
Platelets- 1.4lakhs/cu.mm
Urea- 155mg/dl
Creatinine- 4.7
Uric acid- 7.1
Phosphorus- 2.0
Sodium- 126
Potassium- 2.6
Chloride- 87
ON DAY 4
Hemoglobin- 7.2
TLC- 17,409
Platelet count- 1.5
Urea- 162
Uric acid- 5.0
Sodium- 125
Chloride- 88
ON DAY 5
ON DAY 7
Hb- 7
TLC- 22,000
Platelet count- 26,000
Urea- 144
Creatinine - 4.8
Uric acid-9.1
Phosphorus- 4.8
Sodium- 135
Potassium- 4.3
Chloride- 98
Fasting blood sugar- 149
ON DAY 8
Hb- 6.4
TLC- 14,700
Platelet count- 6000
Urea - 149
Creatinine- 4.4
Uric acid- 9.2
TEMPERATURE CHARTING-
INTERPRETATION-
After one week of use of meropenam the fever spikes have shown a fall and there is no new complaint by patient. The WBC counts have also reduced and patient's condition have been improving
TREATMENT:
Day 1 to Day 3:
INJ. MEROPENEM 500mg IV BD
INJ. ZOFER 4mg IV TID
INJ. PAN 40mg IV OD
IV Fluids- NS,RL @ 100 mL/hr
BP/HR/RR/SpO2 charting
Temp charting 4th hrly
RT feeds- 2nd hrly 100 mL water
Day 4
INJ. MEROPENEM 500mg IV BD
INJ. ZOFER 4mg IV TID
INJ. RANTAC 50mg IV OD
INJ. KCl 2 Amp in 500 mL NS over 4.5 hrs infusion
IV Fluids- NS,RL @ 100 mL/hr
SYP. POTCHLOR 10 mL in 1 glass of water TID
SYP. MUCAINE GEL 10 mL PO TID
7 point profile
BP/HR/RR/SpO2 charting
Temp charting 4th hrly
RT feeds- 2nd hrly 100 mL water
Day 5 to Day 10:
INJ. MEROPENEM 500mg IV BD (Day 6)
INJ. ZOFER 4mg IV TID
INJ. RANTAC 50mg IV OD
INJ. LASIX 40 mg IV BD
IV Fluids- NS,RL @ 100 mL/hr
SYP. MUCAINE GEL 10 mL PO TID
GRBS 7 point profile
INJ.HAI SC TID ACC to GRBS
TAB.DOLO 650 mg SOS
BP/HR/RR/SpO2 charting
Temp charting 4th hrly
Day 11:
INJ. COLISTIN 2.25 MU IV OD(Day 4)
INJ. ZOFER 4mg IV TID
INJ. RANTAC 50mg IV OD
INJ. LASIX 40 mg IV BD
IV Fluids- NS,RL @ 100 mL/hr
SYP. MUCAINE GEL 10 mL PO TID
GRBS 7 point profile
INJ.HAI SC TID ACC to GRBS
TAB.DOLO 650 mg SOS
Day 12:
SDP Transfusion done I/v/o low platelet count
Pre transfusion counts:
Hb:6.2 g/dL
TLC:14700
PLt:6000
Post transfusion counts:
Hb:6.4
TLC:13700
PLt:50000
INJ. COLISTIN 2.25 MU IV OD(Day 5)
INJ. ZOFER 4mg IV TID
INJ. RANTAC 50mg IV OD
INJ. LASIX 40 mg IV BD
IV Fluids- NS,RL @ 100 mL/hr
SYP. MUCAINE GEL 10 mL PO TID
GRBS 7 point profile
INJ.HAI SC TID ACC to GRBS
TAB.DOLO 650 mg SOS















































Comments
Post a Comment