1701006110 CASE PRESENTATION
LONG CASE
55 years old female with shortness of breath
Chief complaints:
55 years old female who is housewife came to the hospital on 10/6/22 with chief complaints of
-Shortness of breath Since 2 days
-Bilateral pedal edema since 2 days
-Decreased urine output since 2 days
Timeline of events:
History of presenting illness:
No history of blood transfusions.
Personal history:
Diet -mixed
Appetite -normal
Sleep -adequate
Bowelmovements-regular
Bladder movements-decreased urinary output since 2days
No known drug or food allergies
No addictions
Family history:
No significant family history
General examination:
After taking consent ,patient is examined in well lit room
Patient is conscious, coherent and cooperative well oriented to time ,place and person
moderately built and moderately nourished
Pallor -present
Icterus -absent
Clubbing -absent
Cyanosis -absent
Generalised lymphadenopathy -absent
Edema -absent
Vitals-
(At the time of admission)
Temperature-afebrile
Pulse rate -106 beats per minute ,regular rhythm ,normal volume,normal character ,no radio radial delay
Blood pressure -160/80mmHg measured in left arm in supine position
Respiratory rate -34 cycles per minute
SpO2- 92 %at room air
Systemic examination:
Respiratory system:
Upper respiratory system - normal
Examination of chest-
Inspection:
Shape of the chest -normal, bilaterally symmetrical
Trachea -central in position
Respiratory movements -normal, bilaterally symmetrical
No scars,sinuses, engorged veins seen on chest wall
Palpation:
No local rise of temperature
No tenderness
All inspectory findings are confirmed
Trachea -central in position
vocal Fremitus - normal
Chest movements - normal ,symmetrical bilaterally
Percussion:
Resonant note heard
Auscultation:
Bilateral air entry present
Normal vesicular breath sounds heard
Bilateral basal crepitations heard
Diffuse wheeze present
Cardiovascular system:
Abdominal examination:
Inspection-
Shape of the abdomen- scaphoid
Umbilicus -normal
All quadrants of abdomen area moving normally
Palpation -
No local rise of temperature
No tenderness
Soft ,non tender
Liver not palpable
Spleen not palpable
Auscultation -
Bowel sounds heard
Serum creatinine-

Ultrasonography -
2D echo-
Provisional diagnosis-
Chronic renal disease with pulmonary edema and metabolic acidosis with denovo diabetes mellitus type-2
Treatment :
Dialysis was done after admission in the hospital
On 10/6/22
1)Inj.LASIX 40mg IV/BD
2)tab.NODOSIS 500mg PO/OD
3)tab.MET-XL 25 mg OD
4)tab.AMLONG 10mgOD
5)cap bio-D PO weekly once
6)tab. SHELCAL 500 mg PO OD
7)inj. Erythropoietin 5000 units weekly once
On 11/6/22
1)Inj.LASIX 40mg IV/BD
2)tab.NODOSIS 500mg PO/OD
3)tab.MET-XL 25 mg OD
4)tab.AMLONG 10mgOD
5)cap bio-D PO weekly once
6)tab. SHELCAL 500 mg PO OD
7)inj. Erythropoietin 5000 units weekly once
8)inj.INSULIN SC according to the GRBS
52 years old male with fever with thrombocytopenia
Case history :
52 years old male who is farmer by occupation came to the hospital on 8/6/22 with chief complaints of
-Fever since 4 days
- abdominal distension since 3days
History of presenting illness:
Patient was apparently a symptomatic 4days back then he developed fever which is low grade, continuous ,not associated with chills &rigors , no aggravating factors ,relieved with medications which was given by local RMP
He developed abdominal distension which is insidious in onset ,progressive type ,not associated with pain
He had decreased appetite since 3days
Before admission in our hospital ,He went to government hospital where he diagnosed with thrombocytopenia (17000 cells/mm3)
No history of rashes ,bleeding tendencies
No history of headache ,vomitings, generalised body pains
No history of loose stools , pain abdomen
No history of weight loss
Past history:
No history of similar complaints in the past
No history of hypertension ,diabetes ,TB,asthma,CVA, CAD
Personal history:
Diet - mixed
Appetite- decreased
Sleep -adequate
Bowel &bladder movements -regular
Addictions -occasional alcoholic (90ml)& toddy
Toddy intake 5days back
Family history:
No similar complaints in the family
No history of hypertension ,diabetes ,TB, asthma, cad
General examination:
After taking consent ,patient is examined in well lit room
Patient is conscious, coherent ,cooperative ,well oriented to time , place , person
Moderately built &moderately nourished
Pallor - absent
Icterus -absent
Cyanosis-absent
Clubbing -absent
No lymphadenopathy and edema
Vitals-
Temperature-now Afebrile but at the time of admission he is febrile.
Pulse-85 bpm
Repiratory rate-20 cpm
Bp-120/80 mmHg measured in supine position,in left upper arm .
Spo2:98%at room air
Grbs-120 mg/dl
SYSTEMIC EXAMINATION-
Abdominal examination-
Inspection-
Shape of abdomen -round and distended
Umbilicus- inverted and central in position
No visible scars and sinuses
No engorged veins .
Palpation-
No local rise of temperature
No tenderness
Inspectory findings are confirmed.
Soft and non tender ,no organomegaly ,
abdomen is distended .
PERCUSSION- dull note heard
AUSCULTATION-
Bowel sounds were heard
No bruit.
Respiratory system-
BAE- Present
Normal vesicular breath sounds
Cardiovascular system -
S1,S2 heard ,no murmurs
CNS: normal ,intact
PROVISIONAL DIAGNOSIS-
*Viral pyexia With thrombocytopenia
INVESTIGATIONS-
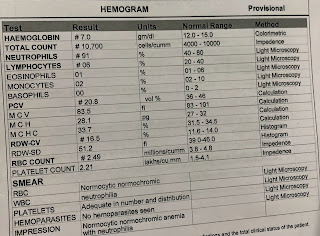
Complete blood picture-
Hb-14.9g%
WBC-10,500 cells/mm3
Platelets-17000/mm3@outside hospital report
On 8/06/22:
Platelets-22000 /cumm
Neutrophils -43%
Lymphocytes -48 %
Eoisinophils -01%
Blood urea-59 mg/dl
Serum creatinine -1.6mg/dl
Serum electrolytes:
Na-142 mEq/l
K-3.9mEq/l
Cl-103 mEq/l
Liver function tests-
Total bilirubin-1.27 mg/dl
Direct bilirubin-0.44 mg/dl
SGOT-60 IU/L
SGPT-47IU/L
ALP-127IU/L
TOtal proteins- 5.9 gm/dl
Albumin-3.5g/dl
A/G ratio-1.48
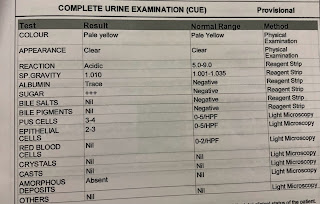
COmplete urine examination-
Albumin -positive
Pus cells -4-5
Epithelial cells -2-3
NS1 ANTIGEN - POSITIVE
SEROLOGY -IgM and IgG negative
on 9/06/22-
Hb- 14.3g%
Platelets- 30,000/cumm
On 10/06/22-
Hb-14.0 g%
Platelets-84000/cumm
USG-
GRADE 2 FATTY LIVER
MILD SPLENOMEGALY
RIGHT SIDE PLEURAL EFFUSION (MILD)
MILD ASCITES
Treatment-
*On 8/6/22
IV FLUIDS - NS AND RL@100ML/hr
Inj.pan 40 mg iv /oD
Inj.optineuron 1 amp in 100 ml Na iv/OD over 30 mins
Inj.zofer 4 mg iv/SOS
VITALS monitoring 4th hourly
*On 9/6/22
Iv fluids - Ns/RL @100 ml/hr
Inj.pan 40 mg iv/OD
Inj.optineuron 1 amp in 100 ml/Ns/iv/OD over 30 mins
Inj.zofer 4mg/iv/sos
Tab.doxycycline 100mg PO/BD
VITALS monitoring
*On 10/06/22;
Iv fluids - NS,RL@100 ml/hr
Inj.pan 40 mg iv/oD
Tab.doxycycline 100 mg Po/BD
Inj zofer 1 amp iv/sos
Inj.optineuron 1 amp in 100 ml Ns/iv/OD over 30 mins
VITALS monitoring 4 th hourly
*On 11/06/22-
Iv fluids - NS,RL@100 ml/hr
Inj.pan 40 mg iv/oD
Tab.doxycycline 100 mg Po/BD
Inj zofer 1 amp iv/sos
Inj.optineuron 1 amp in 100 ml Ns/iv/OD over 30 mins
DOLO 650mg /sos
VITALS monitoring





































Comments
Post a Comment