LONG CASE
22 years old female , daily wage labourer by occupation ,resident of miryalguda was bought to the opd with chief complaints of
• no urine output since 5 days
• generalized edema since 5 days
HISTORY OF PRESENTING ILLNESS :
• Patient is a known case of diabetes mellitus and hypertension. At the age of 10 years, she had fever, increased appetite and increased frequency of micturition for which she was taken to a hospital where she was diagnosed with diabetes.
•She was on oral hypoglycemic agents for 1 year and later she was kept on insulin 2 times a day.
•Later, 2-3 years back she was in altered sensorium for which she was bought to the hospital. She had hyperglycemia and the dose of insulin was increased.
• 20 days back she was bought to the opd with generalized edema , decreased urine output and diagnosed with renal failure and nephrotic syndrome. She was dialysed 5 times and 1 unit of blood transfusion was done. She got discharged.
• She got admitted again for the same
complaints.
• The edema first started around the eyes which was more in the morning and decreased towards the end of the day. Later it progressed to involve the entire body.Decreased urine output since 15 days. Later since 5 days there is no urine output.No hematuria, No loin pain, No history fever or sore throat recently.
PAST HISTORY :
Patient is a known case of diabetes since 12 years and hypertension since 1 year.
No h/o Tb, epilepsy, asthma
No previous surgical history
FAMILY HISTORY :
No history of diabetes or hypertension in the family
PERSONAL HISTORY :
Diet - mixed diet
Appetite - decreased appetite since 6 months
Sleep - adequate
Bowel movements - regular
Bladder movements - normal before 20 days
No addictions
No food or drug allergies
MENSTRUAL AND OBSTETRIC HISTORY :
Attained menarche at the age of 11 years
Regular cycles - 5/30
No pains, No clots
Married 1 year back
2 months of Amenorrhoea 3 months back.
She was pregnant diagnosed based on ultrasound.
On ultrasound , it was found out that there was no cardiac activity of the fetus and she got aborted.
Since then she have no menstrual cycles.
GENERAL EXAMINATION :
Patient is examined in a well lit room after taking the consent.
She is conscious, coherent and cooperative.
Well oriented to time, place and person.
Pallor - present
Icterus - absent
Cyanosis - absent
Clubbing - absent
Generalized Lymphadenopathy - absent
Bilateral pedal edema - present
She has generalized edema ( anasarca)
VITALS :
Pulse - 88 beats per minute, regular in rhythm, normal in volume and character of vessel, no radio- radial delay, no radio - femoral delay.
Respiratory rate - 20 cycles per minute
Blood pressure - 140/80 mm of hg, measured in the left arm in supine position
Temperature - afebrile
Spo2 - 96% at room air
GRBS - 203 mg/dL
SYSTEMIC EXAMINATION :
CVS :
S1 S2 heard, no murmurs
CNS :
No neurological deficit
ABDOMINAL EXAMINATION :
Inspection - abdomen distended
Umbilicus is normal in shape and position
No visible scars or sinuses
No visible gastric peristalsis
No distended veins
Palpation - No local rise of temperature
No tenderness
Organs couldn't be palpated
Percussion - fluid thrill present
Auscultation - bowel sounds normal
RESPIRATORY EXAMINATION :
Examination done in sitting position.
Inspection of URT - normal
Inspection of LRT - Trachea is central in position.
Chest is symmetrical.
Movement of the chest is equal and thoraco- abdominal type of breathing.
Palpation - Trachea is central in position.
Chest is expanding symmetrically.
Vocal fremitus decreased in inframammary, infraaxillary and infrascapular area on both sides.
Percussion - Stony dull note in inframammary, infraaxillary, infrascapular area on both sides.
On tidal percussion, dullness persisted on right side.
Auscultation - Bilateral air entry present.
Normal vesicular breath sounds.
Decreased breath sounds in inframammary, infraaxillary, infrascapular area on both sides.
INVESTIGATIONS :
Hemogram:
Blood urea - 127mg/dL
Serum creatinine - 6.7mg/dL
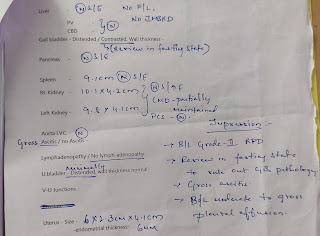
Ultrasound :
Chest Radiograph :
Serum electrolytes :
Sodium - 136 mEq/L
Potassium - 3.5 mEq/L
Chloride - 97 mEq/L
DIAGNOSIS :
Chronic kidney disease on maintenance hemodialysis with bilateral pleural effusion.
TREATMENT :
• Inj. LASIX 60mg/ IV/ BD
• INSULIN INFUSION 6ml / hr
1ml of insulin in 39ml of normal saline
• Tab. NICARDIA 20mg/ PO / BD
• Tab. TELMA 40mg/ PO / BD
• Nil by mouth
• Fluid and salt restriction
• Hourly monitoring of GRBS
-------------------------------------------------------
SHORT CASE
75 years old female home maker by occupation, resident of dhamarcherla was bought to the casuality with chief complaints of vomitings and giddiness since 1 day.
HISTORY OF PRESENTING ILLNESS :
•Patient is a known case of diabetes mellitus and hypertension since 6 years.
•She was apparently asymptomatic 6 years back.
Later she had complaints of headache, generalized weakness for which she was taken to a hospital and there she was diagnosed with diabetes mellitus and hypertension and prescribed on oral medication. From then she was on regular medication.
• Patient did not use oral hypoglycemics and anti- hypertensives for the past 4 days as she went to relatives house.
• Patient presented with 2-3 episodes of vomitings, non- bilious and non - projectile followed which she developed giddiness. Contents of the vomitus are food and it is not foul smelling. No history of fever or pain abdomen.She was taken to a local hospital where it was found out that her GRBS is 394mg/dL and ketone bodies were positive and referred to our hospital.
• No history of shortness of breath, chest pain, palpitations.
PAST HISTORY :
She is a known case of diabetes mellitus and hypertension since 6 years.
No history of Tuberculosis, cardiovascular disease.
Surgical history - history of cataract surgery 3years back in one eye and 2 years back in the other eye.
PERSONAL HISTORY :
Diet - mixed
Appetite - normal
Sleep - adequate
Bowel and bladder movements - regular
Addictions - chutta smoking for 10years , 3 chutta per day and stopped 5 years back.
No allergies
FAMILY HISTORY :
Not significant
MENSTRUAL AND OBSTETRIC HISTORY :
Attained menopause
8 children - 4 boys and 4 girls
GENERAL EXAMINATION :
Patient was examined in a well lit room after taking informed consent.
She was conscious, coherent and cooperative.
Oriented to time, place and person.
Pallor - present
Icterus - absent
Cyanosis - absent
Clubbing - absent
Generalized lymphadenopathy - absent
Bilateral pedal edema - absent
VITALS :
Pulse - 96 beats per minute, irregularly irregular in rhythm, no radio-radial delay, no radio- femoral delay.
Blood pressure - 230/100 mm of hg measured in left arm in supine position
Respiratory rate - 17 cycles per minute
Temperature - Afebrile
GRBS - 393 mg/dL
SYSTEMIC EXAMINATION :
CVS :
Inspection : no visible pulsation , no visible apex beat , no visible scars.
Palpation: apex beat felt.
Auscultation:
Mitral area, tricuspid area, pulmonary area, aortic area- S1,S2 heard.
CNS :
Higher mental functions - Normal
Cranial nerve functions - Normal
Sensory system - Sensitive
Motor system Right. Left
Power- UL 5/5 5/5
LL 5/5 5/5
Tone- UL Normal Normal
LL Normal Normal
Reflexes-
Superficial reflexes - Intact
Plantar flexion flexion
Deep tendon reflexes -
Biceps ++ ++
Triceps ++ ++
Supinator ++ ++
Knee ++ ++
Ankle ++ ++
Gait- Normal
Cerebellar system - intact
RS :
Inspection:
No tracheal deviation
Chest bilaterally symmetrical
Type of respiration: thoraco abdominal.
No dilated veins,pulsations,scars, sinuses.
Palpation:
No tracheal deviation
Vocal fremitus- normal on both sides.
Percussion:
Resonant in all areas
Auscultation:
Normal Vesicular breath sounds
Bilateral Airway entry - present.
ABDOMINAL EXAMINATION :
INSPECTION :
Abdomen - distension present
Umbilicus - normal
Movements - all quadrants are equally moving with respiration
No scars and sinuses
No visible peristalsis
No engorged veins.
PALPATION:
No local rise in temperature and no tenderness in all quadrants
No organomegaly
PERCUSSION :
no shifting dullness
AUSCULTATION :
Bowel sounds are heard and are normal
No bruit.
INVESTIGATIONS :
Haemogram :
Hb - 11.3 g/dL
TLC - 8100
Platelets - 2.67 lakhs
Normocytic normochromic anaemia
Complete urine examination :
Albumin - 2+
Sugar - 4+
Pus cells - 3-6
Epithelial cells - 2-4
RBC - nil
Casts - nil
Urine for ketone bodies - positive
Arterial blood gas analysis :
PH - 7.44
Co2 - 30.6
O2- 71.4
Hco3 - 22.6
O2 Saturation - 94%
Electrolytes :
Sodium - 133 mEq/dL
Potassium - 4.2 mEq/ dL
Chloride - 102 mEq/ dL
Blood urea - 26mg/dL
Serum creatinine - 1mg/dL
Ecg :
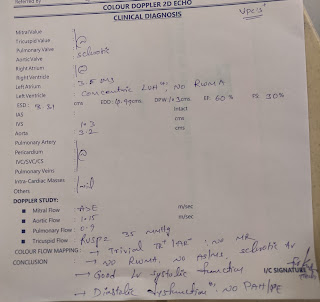
2D echo :
DIAGNOSIS :
Diabetic ketosis with hypertensive urgency
TREATMENT :
• Intra venous fluids( NS, RL) - 100ml /hr
• HUMAN ACTRAPID insulin infusion -6ml/hr
• Tab. NICARDIA 20mg PO/stat
• Inj. OPTINEURON -1 ampoule in 100ml of NS IV/OD
• Inj. ZOFER 4mg IV / TID
• Hourly monitoring of grbs, pulse, bp, rr, and temperature.



75 years old female home maker by occupation, resident of dhamarcherla was bought to the casuality with chief complaints of vomitings and giddiness since 1 day.
HISTORY OF PRESENTING ILLNESS :
•Patient is a known case of diabetes mellitus and hypertension since 6 years.
•She was apparently asymptomatic 6 years back.
Later she had complaints of headache, generalized weakness for which she was taken to a hospital and there she was diagnosed with diabetes mellitus and hypertension and prescribed on oral medication. From then she was on regular medication.
• Patient did not use oral hypoglycemics and anti- hypertensives for the past 4 days as she went to relatives house.
• Patient presented with 2-3 episodes of vomitings, non- bilious and non - projectile followed which she developed giddiness. Contents of the vomitus are food and it is not foul smelling. No history of fever or pain abdomen.She was taken to a local hospital where it was found out that her GRBS is 394mg/dL and ketone bodies were positive and referred to our hospital.
• No history of shortness of breath, chest pain, palpitations.
PAST HISTORY :
She is a known case of diabetes mellitus and hypertension since 6 years.
No history of Tuberculosis, cardiovascular disease.
Surgical history - history of cataract surgery 3years back in one eye and 2 years back in the other eye.
PERSONAL HISTORY :
Diet - mixed
Appetite - normal
Sleep - adequate
Bowel and bladder movements - regular
Addictions - chutta smoking for 10years , 3 chutta per day and stopped 5 years back.
No allergies
FAMILY HISTORY :
Not significant
MENSTRUAL AND OBSTETRIC HISTORY :
Attained menopause
8 children - 4 boys and 4 girls
GENERAL EXAMINATION :
Patient was examined in a well lit room after taking informed consent.
She was conscious, coherent and cooperative.
Oriented to time, place and person.
Pallor - present
Icterus - absent
Cyanosis - absent
Clubbing - absent
Generalized lymphadenopathy - absent
Bilateral pedal edema - absent
VITALS :
Pulse - 96 beats per minute, irregularly irregular in rhythm, no radio-radial delay, no radio- femoral delay.
Blood pressure - 230/100 mm of hg measured in left arm in supine position
Respiratory rate - 17 cycles per minute
Temperature - Afebrile
GRBS - 393 mg/dL
SYSTEMIC EXAMINATION :
CVS :
Inspection : no visible pulsation , no visible apex beat , no visible scars.
Palpation: apex beat felt.
Auscultation:
Mitral area, tricuspid area, pulmonary area, aortic area- S1,S2 heard.
CNS :
Higher mental functions - Normal
Cranial nerve functions - Normal
Sensory system - Sensitive
Motor system Right. Left
Power- UL 5/5 5/5
LL 5/5 5/5
Tone- UL Normal Normal
LL Normal Normal
Reflexes-
Superficial reflexes - Intact
Plantar flexion flexion
Deep tendon reflexes -
Biceps ++ ++
Triceps ++ ++
Supinator ++ ++
Knee ++ ++
Ankle ++ ++
Gait- Normal
Cerebellar system - intact
RS :
Inspection:
No tracheal deviation
Chest bilaterally symmetrical
Type of respiration: thoraco abdominal.
No dilated veins,pulsations,scars, sinuses.
Palpation:
No tracheal deviation
Vocal fremitus- normal on both sides.
Percussion:
Resonant in all areas
Auscultation:
Normal Vesicular breath sounds
Bilateral Airway entry - present.
ABDOMINAL EXAMINATION :
INSPECTION :
Abdomen - distension present
Umbilicus - normal
Movements - all quadrants are equally moving with respiration
No scars and sinuses
No visible peristalsis
No engorged veins.
PALPATION:
No local rise in temperature and no tenderness in all quadrants
No organomegaly
PERCUSSION :
no shifting dullness
AUSCULTATION :
Bowel sounds are heard and are normal
No bruit.
INVESTIGATIONS :
Haemogram :
Hb - 11.3 g/dL
TLC - 8100
Platelets - 2.67 lakhs
Normocytic normochromic anaemia
Complete urine examination :
Albumin - 2+
Sugar - 4+
Pus cells - 3-6
Epithelial cells - 2-4
RBC - nil
Casts - nil
Urine for ketone bodies - positive
Arterial blood gas analysis :
PH - 7.44
Co2 - 30.6
O2- 71.4
Hco3 - 22.6
O2 Saturation - 94%
Electrolytes :
Sodium - 133 mEq/dL
Potassium - 4.2 mEq/ dL
Chloride - 102 mEq/ dL
Blood urea - 26mg/dL
Serum creatinine - 1mg/dL
Ecg :
2D echo :
DIAGNOSIS :
Diabetic ketosis with hypertensive urgency
TREATMENT :
• Intra venous fluids( NS, RL) - 100ml /hr
• HUMAN ACTRAPID insulin infusion -6ml/hr
• Tab. NICARDIA 20mg PO/stat
• Inj. OPTINEURON -1 ampoule in 100ml of NS IV/OD
• Inj. ZOFER 4mg IV / TID
• Hourly monitoring of grbs, pulse, bp, rr, and temperature.



























Comments
Post a Comment