1701006123 CASE PRESENTATION
LONG CASE
75year old female who is a housewife , resident of miryalaguda was brought to the casuality with
CHIEF COMPLIANTS
Giddiness since 1day
Vomiting since 1day .
HISTORY OF PRESENT ILLNESS :
Patient was apparently asymptomatic 6years back and was able to perform her regular activities without any difficulty then she experienced headache and generalised weakness for which she consulted a local medical practitioner and was diagnosed with TYPE 2 DIABETES MELLITUS and HYPERTENSION. She was prescribed with medicines (oral hypoglycemic Agents and antihypertensive drugs) and was on regular medication.
4 days back she went to her relatives house and has a H/O no intake of antihypertensives and oral hypoglycemic drugs due to which she developed vomitings and giddiness.
VOMITINGS -
Sudden in onset
Non bilious , non projectile , non foul smelling.
Food particles as content .
Not associated with fever , pain abdomen and loose stools.
She was taken to the local hospital and was found to have General random blood sugar (GRBS) 394mg/dl.
And also urinary ketone bodies were positive .
No H/O chest pain , palpitations , syncopal attacks.
No H/O shortness of breath , burning micturition .
PAST HISTORY :
No similar compliants in the past.
Not a known case of tuberculosis , Coronary artery disease, epilepsy , asthma .
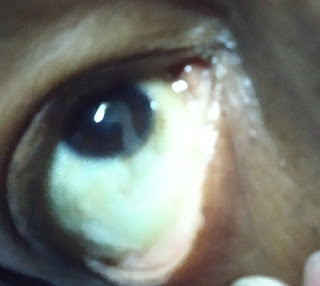
Surgical history : H/O cataract surgery 3 back in right eye and 2 yrs back in left eye .
PERSONAL HISTORY:
Mixed diet
Appetite normal
Sleep adequate
Bowel and bladder regular
Addictions : chutta smoking for 10years , 3 chutta per day and stopped 5 years back.
Intake of alcohol and toddy on social gatherings.
FAMILY HISTORY :
Not significant.
No H/O Tuberculosis, epilepsy, asthma .
GENERAL EXAMINATION :
Patient is conscious, coherent and cooperative ,
well oriented to time, place , person.
Moderately built and nourished.
Patient was examined in supine position in a well lighted room after taking consent.
Pallor - absent
Icterus - absent
Cyanosis - absent
Clubbing - absent
Lymphadenopathy - absent
Edema - absent
VITALS :
Temperature - afebrile
Pulse rate - 90 beats per minute.
Respiratory rate - 20 cycles per minute
Blood pressure - 230/110mmHg at the time of presentation(around 7pm) 09/06/2022.
On 10 /06/2022
Blood pressure - 150/100mmHg.
GRBS - 394mg/dl ( at presentation)
On 10/06/22 - 226mg/dl .
11/06/2022
Blood pressure - 180/100 mm Hg
Pulse rate - 72 beats per minute
SYSTEMIC EXAMINATION ::
GIT
INSPECTION :
Abdomen - distended
Umbilicus - transverse slit like
Movements - all quadrants are equally moving with respiration
No scars and sinuses
No visible peristalsis
No engorged veins.
PALPATION:
No local rise in temperature and no tenderness in all quadrants
LIVER: no hepatomegly
SPLEEN- not enlarged
KIDNEYS - bimanual palpable kidneys
PERCUSSION :
no shifting dullness
AUSCULTATION :
Bowel sounds are heard and are normal
No bruit.
Other system examination :
Respiratory system:
Inspection:
No tracheal deviation
Chest bilaterally symmetrical
Type of respiration: thoraco abdominal.
No dilated veins,pulsations,scars, sinuses.
No drooping of shoulder.
Palpation:
No tracheal deviation
Apex beat- 5th intercoastal space,medial to midclavicular line.
Tenderness over chestwall- absent.
Vocal fremitus- normal on both sides.
Percussion:
Supraclavicular
Infraclavicular.
Mammary
Axillary
Infraaxillary
Suprascapular
Infrascapular
Interscapular
Right side and left side- resonant in above areas.
Auscultation:
Normal Vesicular breath sounds
Bilateral Airway entry - present.
Cardiovascular system:
Inspection : no visible pulsation , no visible apex beat , no visible scars.
Palpation: all pulses felt , apex beat felt.
Percussion: heart borders normal.
Auscultation:
Mitral area, tricuspid area, pulmonary area, aortic area- S1,S2 heard.
Central Nervous system:
Higher motor functions- Normal
Speech: Normal
Cranial nerve functions - Intact.
Sensory system- sensitive to pain, touch , vibration and temperature.
Motor system Right. Left
Power- UL 5/5 5/5
LL 5/5 5/5
Neck Normal
Trunk muscles Normal
Tone- UL Normal Normal
LL Normal Normal
Reflexes-
Superficial reflexes - Intact
Plantar flexion flexion
Deep tendon reflexes -
Biceps ++ ++
Triceps ++ ++
Supinator ++ ++
Knee ++ ++
Ankle ++ ++
Gait- Normal
Cerebellar system - intact
DIAGNOSIS :
HYPERGLYCEMIA AND HYPERTENSIVE URGENCY (2⁰ to non compliance to medication) .
INVESTIGATION:
PROVISIONAL DIAGNOSIS :
DIABETIC KETOSIS WITH HYPERTENSIVE URGENCY.
TREATMENT :
1. I.V fluids (normal saline,ringer lactate) at 100ml/hr.
2. Inj. Human act rapid insulin i.v. infusion at 6ml/hr.
3. Inj.Zofer 4mg i.v. /TID
4. Optineuron 1 ampule in 1000ml NS i.v. OD
5. Nicardia 20mg PO stat.
6. Hourly GRBS , B.P. , vitals monitoring.
7 . Strict I/O charting.
----------------------------------------------------------------------------------------------------------------------------
SHORT CASE
45/m resident of bibinagar came to the casuality
Cheif complaints :
Sob on exertion: 2months
Tingling sensation of limbs: 2 month's
Dark coloured stool :3 days back
HOPI:
Patient was apparently asymptomatic 2 months back den he development sob on exertion which was insidious in onset and gradual in progression.
Not associated with orthopnea and PND, wheeze
Not associated with edema
Tingling sensation in the limbs in both the lowe limbs
Since 2months
Dark colored stool 3 days back.
History of fever and oral ulcers
No history of weight loss ,no loss of appetite
No history of pain abdomen or abdominal distension , vomitings ,loose stools .
No history of burning micturition.
Past History:
No History of similar complaints in the past.
No history of Diabetes , Hypertension , Tuberculosis ,Bronchial asthma ,COPD , coronary artery disease , Cerebrovascular accident ,thyroid disease.
Family History:
No H/o of similar complaints in the family
Personal history :
Diet : mixed
Appetite: decreased
Sleep : adequate
Bowl and bladder : regular
Addiction: Chews pan.
General examination:
Patient is conscious, coherant and cooperative
Moderately built and moderatly nourished
Pallor :++
No icterus, cyanosis, clubbing, lymphadenopathy, generalised edema.
Vitals
Patient is afebrile .
Pulse - 90 beats / min ,normal voulme ,regular rhythm,normal character ,no radiofemoral delay,radioradial delay.
BP - 110/80 mmhg ,measured in supine position in both arms .
Respiratory rate -16breaths / min.
Systemic examination
Respiratory system:
Inspection:
No tracheal deviation
Chest bilaterally symmetrical
Type of respiration: thoraco abdominal.
No dilated veins,pulsations,scars, sinuses.
No drooping of shoulder.
Palpation:
No tracheal deviation
Apex beat- 5th intercoastal space,medial to midclavicular line.
Tenderness over chestwall- absent.
Vocal fremitus- normal on both sides.
Percussion:
Supraclavicular
Infraclavicular.
Mammary
Axillary
Infraaxillary
Suprascapular
Infrascapular
Interscapular
Right side and left side- resonant in above areas.
Auscultation:
Normal Vesicular breath sounds.
Bilateral Airway entry - present.
Cardiovascular system:
Inspection : no visible pulsation , no visible apex beat , no visible scars.
Palpation: all pulses felt , apex beat felt.
Percussion: heart borders normal.
Auscultation:
Mitral area, tricuspid area, pulmonary area, aortic area- S1,S2 heard.
GIT
INSPECTION :
Abdomen - distended
Umbilicus - transverse slit like
Movements - all quadrants are equally moving with respiration
No scars and sinuses
No visible peristalsis
No engorged veins.
PALPATION:
No local rise in temperature and no tenderness in all quadrants
LIVER: no hepatomegly
SPLEEN- not enlarged
KIDNEYS - bimanual palpable kidneys
PERCUSSION :
no shifting dullness
AUSCULTATION :
Bowel sounds are heard and are normal
No bruit.
CNS:
Higher motor functions- Normal
Speech: Normal
Cranial nerve functions - Intact.
Sensory system- sensitive to pain, touch , vibration and temperature.
Motor system Right Left
Power- UL 5/5 5/5
LL 5/5 5/5
Neck Normal
Trunk muscles Normal
Tone- UL Normal
LL Normal
Reflexes-
Superficial reflexes - Intact
Plantar flexion flexion
Deep tendon reflexes -
Biceps ++ ++
Triceps ++ ++
Supinator ++ ++
Knee ++ ++
Ankle ++ ++
Gait- Normal
Cerebellar system - intact
Investigation:
Provisional Diagnosis: pancytopenia 2 to B 12 defici
ency.
Treatment:
1) Inj. vitocofol. 1000mcg
2) Tab.Pain D
3) Inj. Optineuron.


















Comments
Post a Comment