1701006133 CASE PRESENTATION
LONG CASE
A 65yr old male patient who is a resident of nakrekal and farmer by occupation came to the OPD with the chief complaints of
Urinary retention since 2 days
Abdominal distention since 2 days
Fever since 3 days
HISTORY OF PRESENT ILLNESS:
PAST HISTORY
He had right sided indirect inguinal hernia for which hernioraphy was done 13 years back.
He is known case hypertension since 4 years and he is on medication since 4 years
No history of diabetes,asthma,tb,cad,stroke
PERSONAL HISTORY
married
Diet:mixed
Appetite:normal
Sleep:adequate
Bowel and bladder:urinary retention
Addictions:regular alcoholic
FAMILY HISTORY:
family member has hypertension
No history of diabetes,asthma,tb,cad,stroke.
GENERAL EXAMINATION
Patient is concious,coherent,cooperative,moderately built and moderately nourished
VITALS:
Temperature:98.7°F
Pulse rate:82b/m
Respiratory rate:22c/m
BP:140/70mmhg
Spo2:99
Grbs:134mg%
Pallor: present
Icterus:no
Clubbing:no
Cyanosis:no
Lymphadenopathy:no
Edema:present
SYSTEMIC EXAMINATION:
Shape:scaphoid
Umbilicus:central,inverted
Skin:normal
Dilated veins:no
No visible gastric peristalsis
Movements of abdominal wall:normal
PALPATION:
SUPERFICIAL PALPATION:
No Tenderness
No local rise of temperature
DEEP PALPATION:
liver:not palpable
Spleen:not palpable
Kidney:not palpable
PERCUSSION:
Fluid thrill:absent
Liver span:14cm
AUSCULTATION:
Bowel sounds:normal
EXAMINATION OF OTHER SYSTEMS:
CARDIOVASCULAR SYSTEM:
S1,S2 Heard
no added heart sounds
RESPIRATORY SYSTEM:
broncho vesicular breath sounds heard
CNS EXAMINATION:
Tab nodosis-500mg bd
Inj metrogel-500mg tid
Tab pan- 40mg OD
Oroferxt- OD
Tab shelcal-od
Tab nicardipine-20mg bd
-------------------------------------------------------
SHORT CASE
29 YEARS OLD FEMALE WITH COMPLIANTS AND DURATION:
PIGMENTATION OVER FACE-6 MONTHS
HAIR FALL FROM SCALP- 6MONTHS
HISTORY OF LOSS OF APPETITE
HISTORY OF FEVER-6 MONTHS
HISTORY OF JOINT PAIN:6MONTHS
HISTORY OF MORNING STIFFNESS
HISTORY OF PEDAL EDEMA
HISTORY OF ULCERS IN ORAL CAVITY:5MONTHS
HOPI :
PATIENT WAS APPARENTLY ASYMPTOMATIC BEFORE 15 NOVEMBER 2021.
ON 15 NOVEMBER 2021 PATIENT STARTED DEVELOPING FEVER , SWELLING AT SYNOVIUM OF ANKLE JOINT WHICH LATER LEAD TO PEDAL EDEMA AND ASSOCIATED WITH REDUCED PLATELET COUNT FOR WHICH SHE WAS TAKEN TO A NEARBY HOSPITAL WHERE SHE RECEIVED THE TREATMENT AND LATER DURING THE HOSPITAL STAY SHE DEVELOPED PAIN IN ALL JOINTS ASSOCIATED WITH SWELLING AND EARLY MORNING STIFFNESS SINCE THEN. ALSO DEVELOPED PIGMENTATION OVER FACE , SCALP, BOTH EARS , NECK, BOTH HANDS AND LEGS, ARMS AND FOREARMS FOLLOWING WHICH SHE DEVELOPED ORAL ULCERS, THROAT PAIN WHICH IS ON AND OFF , THINNING OF HAIR AND HAIRFALL
PAST HISTORY :
HISTORY OF ABORTION
HISTORY OF SEZIURES
NO HISTORY OF DIABETES MELLITUS
NO HISTORY OF HTN
PREVIOUS SURGERIES : HYSTERECTOMY
PERSONAL HISTORY :
DIET : MIXED
APPETITE : REDUCED
SLEEP : INADEQUATE
BOWEL AND BLADDER : REGULAR
GENERAL EXAMINATION:
PATIENT IS C/C/C
NO PALLOR, ICTERUS , CYANOSIS
BILATERAL PEDAL EDEMA +
VITALS :
BP - 110 / 70 mmhg
PR - 98 bpm
SPO2 - 99% @RA
TEMP - FEVER SPIKES
SYSTEMIC EXAMINATION :
CVS - S1 S2 +
RS - BAE +
CNS : NAD
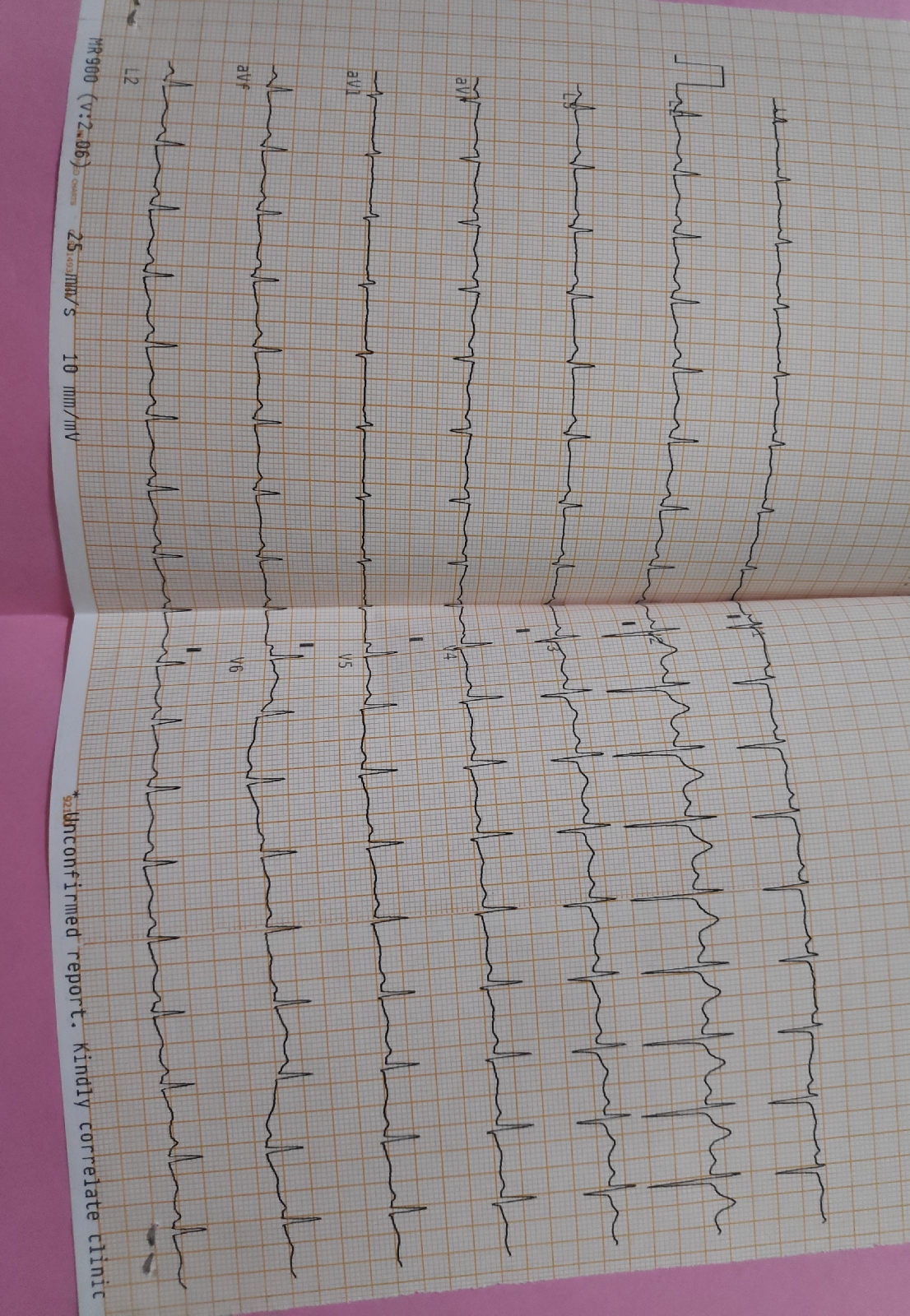
INVESTIGATIONS
ECG:
PROVISIONAL DIAGNOSIS : SYSTEMIC LUPUS ERYTHEMATOSUS .
TREATMENT :
31/5/2022
PHOTO BAN CREAM (TID)
TAB CLONAZEPAM 0.5MG
2/6/2022:
TAB ULTRACET1/2 TAB OID
WYSOLONE 20MG OD
TAB HCQ 10MGBD
6/6/2022:
TAB ULTRACET 1/2 TAB OD
TAB HCQ 10MG BD
ING NEOMAL 1G I. V
TAB WYSOLONE:20 MG OD




































Comments
Post a Comment