1701006137 CASE PRESENTATION
LONG CASE
CHIEF COMPLAINS:
The patient was apparently asymptomatic 6 months ago when he developed jaundice and was treated at a private practitioner.
Later he developed abdominal distension about 7 days ago which was insidious in onset, gradually progressive to the present size and is associated with
- Pain in epigastric and right hypochondric region which was also insidious in onset and gradually progressive,without any aggrevating or releiving factors
It was colicky type.
- Fever - high grade ,continuous , not associated with chills and rigor, decreased on medication, No night sweats.
- Not associated with Nausea, vomiting, loose stools
He also complains of pedal edema which was insidious in onset ,gradually progressive ,bilateral pitting type,which is present below the knees {grade-2}
- Increases during the day - maximum at evening.
- No local rise of temperature and tenderness
- Not relived on rest
He also complained of shortness of breath since 4 days - progressed to MMRC grade 4,it was insidious in onset,gradually progressive which aggrevated on eating and lying down,no relieving factors.
- No PND
- No cough/sputum/hemoptysis
- No chest pain
- No wheezing
Daily Routine :
Wakes up at 5am and goes to field.
Comes home at 8am and has rice for breakfast. Returns to work at 9am.
1pm - lunch
2-6 pm - work
6pm - home
8pm - dinner
Alcohol- 2 times a week, 180 ml.
PAST HISTORY:
No history of similar complaints in the past
Medical history- not a known case of DM, HTN, TB, Epilepsy, Asthma, CAD
No surgical history
PERSONAL HISTORY:
Mixed diet
Reduced appetite since 7 days
Sleep is disturbed due to breathlessness
Bowel movements are regular
Bladder - oliguria since 2 days, no burning micturition, no feeling of incomplete voiding.
No known Allergies
Addictions - Beedi - 8-10/day since 20 years ;
- Alcohol - Toddy - 1 bottle, 2 times a week, since 20 years;
- Whiskey-180 ml, 2 times a week, since 5 years.
- Last alcohol intake - 29th May, 2022 , amount : more than usual.
FAMILY HISTORY:
No similar complains in the family
GENERAL EXAMINATION:
Examined in a well lit room with proper consent
Patient is conscious, coherent and co-operative.
Moderately built and nourished
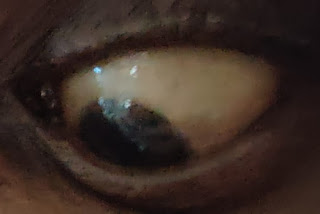
Icterus - present (sclera)
Pedal edema - present - bilateral pitting type, grade 2
No pallor, cyanosis, clubbing, lymphadenopathy.
Vitals :
Temperature- afebrile
Respiratory rate - 14 cpm
Pulse rate - 98 bpm
BP - 120/80 mm Hg.
SYSTEMIC EXAMINATION:
CVS : S1 S2 heard, no murmurs
Respiratory system : normal vesicular breath sounds heard.
Abdominal examination:
INSPECTION :
Shape of abdomen- distended
flanks -full
Umblicus - everted and central.no herniations present
Movements of abdominal wall - moves with respiration
Skin is smooth and shiny;
No scars, sinuses, distended veins, striae.
PALPATION :
Local rise of temperature is present .
Tenderness is present in the epigastric region.
No Hepatomegaly and splenomegaly
Guarding present(volunatary contraction of abdominal wall musculature to avoid pain)
Rigidity absent(involuntary tightening of abdominal muscles)
No visible peristalsis
Fluid thrill positive
Liver not palpable
Spleen not palpable
Kidneys not palpable
Lymph nodes not palpable
PERCUSSION:
Liver span : not detectable
Fluid thrill: felt
AUSCULTATION:
Bowel sounds: heard in the right iliac region
No bruit present
CNS EXAMINATION:
Conscious
Speech normal
No signs of meningeal irritation
Cranial nerves: normal
Sensory system: normal
Motor system: normal
Reflexes: Right. Left.
Biceps. ++. ++
Triceps. ++. ++
Supinator ++. ++
Knee. ++. ++
Ankle ++. ++
Gait: normal
INVESTIGATIONS:
- Hemogram :
Hemoglobin : 9.8 g/dl
TLC : 7,200
Neutrophils : 49%
Lymphocytes : 40%
Eosinophils : 1%
Basophils : 0%
PCV : 27.4%(40-50)
MCV : 92.3 fl
MCH : 33 pg
MCHC : 35.8%
RDW-CV : 17.6%
RDW-SD : 57.8 fl
RBC count : 2.97 millions/mm3
Platelet count : 1.5 lakhs/mm3
Smear : Normocytic normochromic anemia
- LFTs :
Total Bilirubin : 2.22 mg/dl (0-1)
Direct Bilirubin : 1.13 mg/dl(0-0.2)
AST : 147 IU/L(0-35)
ALT : 48 IU/L(0-45)
ALP : 204 IU/L(53-128)
Total proteins : 6.3 g/dl(6.4-8.3)
Serum albumin : 3 g/dl(3.5-5.2)
A/G ratio : 0.9
- ESR :
15mm/1st hour
- Prothrombin time : 16 sec
- APTT : 32 sec
- Serum electrolytes :reduced
Sodium : 133 mEq/L(136-145)
Potassium : 3 mEq/L(3.5-5.1)
Chloride : 94 mEq/L(98-107)
- Blood Urea : 12 mg/dl
- Serum Creatinine : 0.8 mg/dl
- Ascitic fluid :
Protein : 0.6 g/dl(<2.5)
Albumin : 0.34 g/dl
Sugar : 95 mg/dl (60-100)
LDH : 29.3 IU/L (230-460)
SAAG : 2.66 (<1.1)
- Serology :
HbsAg : Negative
HCV : Negative
HIV : Negative
PROVISIONAL DIAGNOSIS:
This is a case of Decompensated Chronic liver failure with ascites which may be secondary to chronic alcohol consumption.
TREATMENT:
Fluid restriction less than 1L per day
Salt restriction less than 2 gm per day
Inj. Pantoprazole 40 mg IV OD
Inj. Lasix 40 my IV BD
Tab. Spironolactone 50 mg BB
Inj. Thiamine 1 Amp in 100 ml IV TID
Syrup Potchlor 10ml PO TID
Syp. Lactose 15ml TID
Ascitic fluid tapping was done.
CHIEF COMPLAINS:
HISTORY OF PRESENTING ILLNESS:
PAST HISTORY:
PERSONAL HISTORY :
FAMILY HISTORY:
GENERAL EXAMINATION:
Examined in a well lit room with proper consent
Patient is conscious, coherent and co-operative.
Moderately built and nourished.
Truncal obesity is present.
No pallor , icterus, cyanosis, clubbing, lymphadenopathy and edema.
Vitals:
Temperature- Afebrile
Respiratory rate - 18cpm
Pulse rate- 165bpm
Blood pressure- 110/80mmhg
SPO2-98%
GRBS-132mg/dl post prandil









.jpeg)
.jpg)







.jpeg)
.jpeg)

.jpeg)
.jpeg)

.jpeg)


Comments
Post a Comment