LONG CASE :
Chief complaints:
55 years old female who is housewife came to the hospital on 10/6/22 with chief complaints of
-Shortness of breath Since 2 days
-Bilateral pedal edema since 2 days
-Decreased urine output since 2 days
TIMELINE OF EVENTS:-
HISTORY OF PRESENTING ILLNESS:-
Patient was apparently asymptomatic six years back
Then developed pedal edema which is bilateral ,for which she visited hospital and diagnosed with hypertension and renal failure
And on conservative management
From past 2days,
—patient developed shortness of breath grade 4 sudden in onset, not associated with chest pain ,sweating .
No orthopnea & pnd , cough
—Bilateral pedal edema which is pitting type
—Decreased urinary output not associated with burning micturition
Past history:
Known case of hypertension since 6years
Known case of chronic kidney disease since 6 years
diabetes mellitus type -2( diagnosed after coming to our hospital) — GRBS 418mg%
Not a known case of Asthma,TB ,CAD, epilepsy
No history of surgeries in the past
No history of blood transfusions.
Personal history:
Diet -mixed
Appetite -normal
Sleep -adequate
Bowelmovements-regular
Bladder movements-decreased urinary output since 2days
No known drug or food allergies
No addictions
Family history:
No significant family history
General examination:
After taking consent ,patient is examined in well lit room
Patient is conscious, coherent and cooperative well oriented to time ,place and person
moderately built and moderately nourished
Pallor -present
Icterus -absent
Clubbing -absent
Cyanosis -absent
Generalised lymphadenopathy -absent
Edema - present
VITALS:-
Temperature-afebrile
Pulse rate -106 beats per minute ,regular rhythm ,normal volume,normal character ,no radio radial delay
Blood pressure -160/80mmHg measured in left arm in supine position
Respiratory rate -34 cycles per minute
SpO2- 92 %at room air
Video showing pitting edema
https://youtu.be/W7ibsTmux8Q
Systemic examination:
Respiratory system:
Upper respiratory system - normal
Examination of chest-
Inspection:
Shape of the chest -normal, bilaterally symmetrical
Trachea -central in position
Respiratory movements -normal, bilaterally symmetrical
No scars,sinuses, engorged veins seen on chest wall
Palpation:
No local rise of temperature
No tenderness
All inspectory findings are confirmed
Trachea -central in position
vocal Fremitus - normal
Chest movements - normal ,symmetrical bilaterally
Percussion:
Resonant note heard
Auscultation:
Bilateral air entry present
Normal vesicular breath sounds heard
Bilateral basal crepitations heard
Diffuse wheeze present
Cardiovascular system:
Inspection-
No raised JVP
The chest wall is bilaterally symmetrical
No dilated veins, scars or sinuses are seen
Palpation-
Apex beat is felt in the fifth intercostal space, 1 cm medial to the midclavicular line
No parasternal heave felt
Percussion-
Right and left borders of the heart are percussed
Auscultation-
S1 and S2 heard, no added thrills and murmurs are heard
Abdominal examination:
Inspection-
Shape of the abdomen- scaphoid
Umbilicus -normal
All quadrants of abdomen area moving normally
Palpation -
No local rise of temperature
No tenderness
Soft ,non tender
Liver not palpable
Spleen not palpable
Kidney not palpable
Auscultation -
Bowel sounds heard
Central nervous system examination-
Higher mental functions -normal
Cranial nerves-Normal
Sensory and motor examination- normal
Reflexes-normal
Investigations
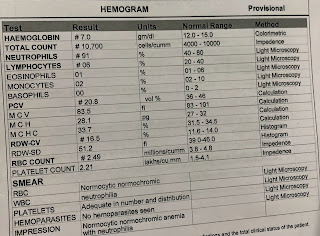
Complete blood picture-
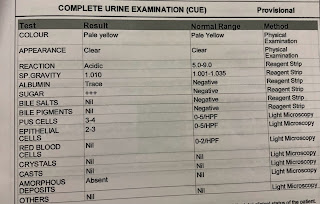
Complete urine examination-
Renal function tests-
Urea - 100mg/dl
Creatinine- 4.2 mg/dl
Arterial blood gas
Bicarbonate- 16.6 mmol/L
Serum electrolytes-
Spot urine sodium -
Urine protein/creatinine ratio-
Liver function tests-
ALP - 442 IU/L
Serum creatinine- 7.1mg/dl
Blood urea- 202 mg/dl

APTT-

Urine for ketone bodies-

Prothrombin time-
Serology-
Ultrasonography -
Right Grade 3 RPD
Left Grade 2 RPD
PROVISIONAL DIAGNOSIS :
Chronic renal disease with pulmonary edema and metabolic acidosis with denovo diabetes mellitus type-2
Treatment:- Dialysis was done after admission in hospital
1)Inj.LASIX 40mg IV/BD
2)tab.NODOSIS 500mg PO/OD
3)tab.MET-XL 25 mg OD
4)tab.AMLONG 10mgOD
5)cap bio-D PO weekly once
6)tab. SHELCAL 500 mg PO OD
7)inj. Erythropoietin 5000 units weekly once
8)inj.INSULIN SC according to the GRBS
On 11/06/22-
Arterial blood gas-
Complete blood picture -
ECG:
12/06/22
fasting blood sugar
--------------------------------------------------------
SHORT CASE
A 22yr old male pt. painter by occupation resident of nalgonda came with
Chief Complaints:
Pain abdomen since 4 days.
HOPI:
Pt. Has started consuming alcohol 4 yrs back due to peer pressure , intially taking one peg per day which has increased to 90ml morning and evening i. e twice daily. He has stopped consuming alcohol 3 months back as advised by the doctor.
Pt. Has history of smoking since 2 yrs . He has been smoking beedies 5 per day till date.
Pt was apparently asymptomatic 3 months back then he developed abdominal pain which was dragging in character for which he was admitted in near by hospital in nalgonda . He was diagnosed with acute pancreatitis and was treated inadequately and was advised to stop consumption of alcohol.
Since then pt has stopped consuming alcohol and has been experiencing alcohol withdrawal symptoms like getting angry , agitation , irritability , craving to consume alcohol, tremors . Pt had consumed alcohol 4 days back due to family problems.
In veiw of this symptoms pt.has been brought to psychiatry OPD for deaddiction. He was referred to medicine OPD in veiw of pain abdomen.
Pain was , insidious in onset , started after consuming of alcohol in epigastrium and left hypochondrium which was relieved on bending forward and lying down , aggrevated on eating food and standing straight.
No h/o fever , nausea , vomiting.
Past history:
H/o similar complaint in past 3 months back.
No other co morbid conditions
No h/o previous medical surgical history.
Family History
Not significant
Diet : mixed
Appetite : normal
Bowel bladder: regular
Sleep: inadequate
GENERAL EXAMINATION
Pt was concious coherent and cooperative
Thin built and moderately nourished

ABDOMEN


No icterus,cyanosis , clubbing,lymphadenopathy, edema
Vitals
Temperature- afebrile
Pulse rate-94bpm
Blood pressure-120/80mmHg
Respiratory rate- 16cpm
Systemic examination:
Abdominal examinations:
Inspection:
Okay Shape of the abdomen- flat
Umbilicus is central
No visible scars,pulsations, peristalsis, engorged veins
Palpation:
All the inspectory findings are confirmed.
Tenderness present over the epigastrium region
No organomegaly
Percussion
No free fluid
Ascultation:
Bowel sounds heard
Other systems:
Respiratory:
b/l air entry present , no added breath sound
CVS :
S1 S2 heard , no added murmurs
CNS :
Higher function intact
No motory and sensory deficit.
Cranial nerves normal .
Investigations
Complete blood picture
Complete urine examination
RFT
USG abdomen
Serum amylase
Serum lipase
Diagnosis:
Pseudocyst of pancreas
secondary to acute pancreatitis.
TREATMENT
Nil per oral
IV fluids Ringer lactate
,Normal saline 100 ml per hour
Inj. Tramadol100mg in 100ml NS IV BD
Inj.pantop 40 mg IV OD
Inj. Optineurin 1 ampoule in 100ml NS IV OD
Psychiatry medication
Tab . Lorazepam 2mg BD
Tab . Benzothiamine100mg OD
12/06/22 FOLLOW UP
VITALS
pulse rate: 92 bpm
BP: 110/70mm of hg
Temp: afebrile
CVS: S1S2 heard
CNS: NAD
Lungs: BAE+
TREATMENT
IV Fluids RL/NS at the rate 75/min
Allow soft diet orally
Continue same medications as above










































Comments
Post a Comment