1701006162 CASE PRESENTATION
LONG CASE:
A 75 years old female, resident of nalgonda, came to casualty on 9th June 2022 with
CHIEF COMPLAINTS:
Vomiting and giddiness since morning.
HISTORY OF PRESENT ILLNESS:
Patient was apparently asymptomatic 6 years back then she had complaints of headache and generalised weakness, for which she visited hospital was diagnosed with type 2 diabetic mellitus and hypertension. She used medication for the same.( Glimepiride 1mg and metformin 500mg)
PAST HISTORY:
PERSONAL HISTORY:
- Diet:mixed
- Appetite: normal
- Sleep: adequate
- Bowel and bladder movements: regular
- Addictions:Consumes alcohol occasionally (90mL), smoked chutta for 10years, stopped 5 years back
- No history of allergies
FAMILY HISTORY:
GENERAL EXAMINATION:
SYSTEMIC EXAMINATION:
- Respiratory system: Normal vesicular breath sounds heard.
- CVS: S1 and S2 heard, no murmurs.
- CNS: no focal neural deficit
- Per Abdomen: soft, non tender, no abdominal mass.
INVESTIGATIONS:
- Random blood sugar: 164mg/dl
- Blood Urea: 26mg/fl
- Serum Creatinine: 1.0 mg/dl
- Electrolytes: Sodium - 139mEq/L Potassium- 3.3mEq/L. Chloride -98mEq/L
- Complete urine examination:
- Albumin: ++
- Sugar: ++++
- Pus cells: 3-6 /HPF
- Epithelial cells: 2-4 / HPF
- Red blood cell: NIL
- Casts: NIL
- Hemoglobin: 11.3mg/dl
- Total leucocyte count: 8900cell/cumm
- Neutrophils: 80
- Lymphocytes:13
- Eosinophils:02
- Monocytes:05
- Platelets: 2.67 lakhs/cumm
- RBC: 4.47million/cumm
- Total bilirubin: 0.74mg/dl
- Direct bilirubin: 0.18mg/dl
- Aspartate transaminase: 29IU/L
- Alkaline phosphate: 143IU/L
- Alanine transaminase: 11IU/L
- Total proteins: 7.7g/dl
- Albumin: 4.1g/dl
- A/G ratio: 1.16
- pH : 7.44
- pCO2 : 30.6mmHg
- pO2. :71.4mmHg
- HCO3:22.6mmol/L
- O2sat:93.8%
PROVISIONAL DIAGNOSIS:
TREATMENT:
- Intravenous fluids normal saline/ ringer lactate @100ml/hr
- Injection Human actrapid insulin I.V infusion @6ml/hr
- Inj. OPTINEURON 1 ampoule in 100ml NS (IV)/ OD
- Inj. ZOFER 4mg IV/ TID
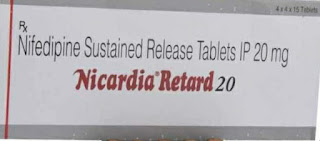
- Tab. NICARDIA 20mg PO/ STAT
- Monitor GRBS, PR, BP, RR CHARTING hourly
- Intravenous fluids NS 2 @ 100ML/hr
- Injection Human actrapid insulin I.V infusion @6ml/hr
- Inj. OPTINEURON 1 ampoule in 100ml NS (IV)/ OD
- Inj. ZOFER 4mg IV/ TID
- Tab TELMA- AM (40/5) mg PO OD
- MONITORING GRBS,BP,PR, RR CHARTING
- Intravenous fluids NS 2 @ 75mL/hr
- Injection Human actrapid insuin 10/10/10 and NPH 8/-/8 ,strict GRBS monitoring
- Inj. OPTINEURON 1 ampoule in NS (IV)/ OD
- Inj. ZOFER 4mg IV/ TID
- Tab CINOD-T (40/10) mg PO OD
- MONITORING BP 2nd hourly charting
-----------------------------------------------------------------------------------------------------------------------------
SHORT CASE:
A 52 year old male, resident of Nalgonda, farmer by occupation, came to hospital with
CHIEF COMPLAINTS:
Fever and abdominal tightness since 6 days
HISTORY OF PRESENTING ILLNESS:
Patient was apparently asymptomatic 6 days ago when he developed,
1.Fever- insidious in onset and gradually progressing, low grade and continuous, not associated with chills and rigor. No aggravating factor and relieved with medication given by local rmp doctor.
2.Abdominal tightness- insidious in onset,not associated with pain ,vomiting and diarrhoea. He also complaints of weakness since 6 days and decreased appetite since 5 days.
He was admitted into Nalgonda hospital for 2 days before getting admitted here he was diagnosed with thrombocytopenia with 17,000cells/mm³
No history of headache,joint pains,body pains.No history of rashes and bleeding tendencies.No history of weight loss.
PAST HISTORY:
No similar complaints in the past.
No history of diabetes mellitus, hypertension, tuberculosis, asthma and epilepsy
PERSONAL HISTORY:
- Diet - Mixed.
- Appetite- decreased since 5 days.
- Sleep - adequate.
- Bowel and bladder- regular.
- Addictions: consumes Alcohol and toddy since 15 years.(consumed toddy i 5 days back)
FAMILY HISTORY:
No similar complaints in past.
No history of asthma, Diabetes mellitus, Hypertension and epilepsy.
GENERAL EXAMINATION:
Patient was examined in a well lit room after taking informed consent. He is conscious, coherent and cooperative; moderately built and well nourished.
No pallor, icterus, cyanosis, clubbing, lymphadenopathy, edema.
VITALS:
- Pulse - 90 beats per minutee
- Respiratory rate - 20 cycles per minute.
- Temperature - afebrile.
- Blood pressure - 120/80 mmHg.
- Spo2 - 98%.
- GRBS - 110 mg/dl.
Right eye:
SYSTEMIC EXAMINATION:
- ABDOMINAL EXAMINATION:
- INSPECTION:
- Abdomen shape - distended
- Flanks full
- Umbilicus - normal
- No visible scars, sinuses , striae , engorged veins.
- No visible gastric peristalsis.
- PALPATION:
- No local rise of temperature.
- No tenderness.
- Abdomen distended.
- Organs not palpable
- PERCUSSION: Fluid thrill is present.
- AUSCULTATION:
- Normal bowel sounds heard.
- No bruit.
- BAE Present.
- Normal vesicular breath sounds heard.
INVESTIGATION:
- Hemogram:
- Hemoglobin - 14.9 gm/dl.
- Total leucocyte count- 10,500cells/ mm³.
- Neutrophils- 43%
- Lymphocytes- 48%.
- Eosinophils - 01%.
- Platelet count - 22000 cells/ cumm.
- PCV - 42.2
- Na:142 mEq/l
- K:3.9mEq/l
- Cl:103 mEq/l
- Total bilirubin-1.27 mg/dl
- Direct bilirubin-0.44 mg/dl
- AST-60 IU/L
- ALT-47 IU/L
- ALP-127IU/L
- Total proteins- 5.9 gm/dl
- Albumin-3.5g/dl
- A/G ratio-1.48
- Albumin ++
- Pus cells - 4-6
- Epithelial cells - 2 -3.
- NS1 ANTIGEN Test - Positive.
- IgM and IgG - Negative.
- Mild splenomegaly .
- On right side mild pleural effusion.
- Mild ascites.
- Grade 2 fatty liver.
- Gall bladder wall - edematous.
- Hemoglobin: 14.3gm/dl.
- Wbc - 8200 cells/cumm
- Neutrophils - 38%
- Lymphocytes-51%.
- Platelet count - 30,000/cumm.
- PCV - 42.0
- Hemoglobin- 14 gm/ dl
- Tlc - 5680cells/cumm.
- Neutrophils -35%
- Lymphocytes - 54%.
- Platelet count-84,000/cumm.
- Wbc- 4800 cells/cumm.
- Neutrophils - 40%
- Lymphocytes-48%
- Platelet count -60,000cells/cumm
- Platelet count -76000cell/cumm.(Same day evening)
- Hb-15.3
- Wbc - 7,100.
- Neutrophils - 40%
- Lympocytes -50%
- Platelet count- 1 lakhcells/cumm.
- PCV - 44.6
PROVISIONAL DIAGNOSIS:
TREATMENT:
- Ivf NS/RL/DNS continuous at 100ml/hr
- Inj. PAN 40mg IV BD
- inj. ZOFER 4mg IV/SOS
- Inj. NEOMOL 1gm IV/SOS
- Tab. PCM 650 mg PO/ SOS
- Inj. OPTINEURON 1 Ampoule in 100ml NS IV/OD over 30mins.
- Oral Fluids
- Tab.dolo650mg/po/sos.
- Tab.pan 10mg/po/od.
- Tab.doxycycline 100mg/po/bd.
- Tab.zincovit po/od
- Vitals monitoring.
















Comments
Post a Comment