1701006163 CASE PRESENTATION
LONG CASE:
A 60 year old female who is a resident of Narsimpeta and an agricultural labourer was brought to the casualty with chief complaints of multiple episodes of loose stools and vomiting with fever for the past 10 days.
History of presenting illness
May,2022: The patient experienced a significant loss in weight that was noticed by herself and her daughter that started sometime during the month of May. She complains of a change in the size of her clothes and says that they are all now loose.
May 2nd,2022: Starting this day and for the next 22 days, the patient consumed 1 bottle of Toddy each day that she shared with her granddaughter. She diluted the toddy with water before consumption.
June 1st ,2022: She reports feeling extremely gassy owing to which she stopped drinking toddy. She complained of abdominal pain that rose till her chest and was relieved by burping.
June 3rd,2022: The patient had 10 episodes of watery diarrhea that was assosciated with abdominal pain. This went on for 4 days. She also had a fever,as reported by her daughter.
June 7th-June 11th,2022: Her symptoms were relieved with no treatment. The symptom free interval lasted for 5 days.
June 12th,2022: The patient once again had 4 episodes of watery diarrhea during the day. This was followed by 2 episodes of vomiting at night. The vomit was not bilious and non projectile in nature. The diarrhea was not bloody. She was taken to the hospital by her daughter where she is currently admitted.
June 13th,2022: As of this day, the patient reports having 5 episodes of watery diarrhea. The diarrhea is preceeded by a migrating abdominal pain which is relieved after passing stools. The pain is worsened by consumption of even small quantities of food or water.
No H/o blood in stools or vomitus, hematuria, burning micturition
No H/o deviation from regular diet or intake of non homemade food in the past 15 days.
The patient traces her finger over her abdomen to show the typical movement of her pain. The pain starts with the onset of meals and ultimately migrates below the umbilicus, ending in a sudden urge to defecate. The pain is relieved by passage of stools, although she feels tenesmus.
Past history:
- She is not a known case of Diabetes, Hypertension, Asthma, CAD, hypothyroidism, TB, RA.
- No drug history.
- No history of other recent illnesses.
Daily routine:
The patient lives with her 7 year old granddaughter. She wakes up at 4am everyday, finishes her household chores and leaves to work at 8am. She has lunch at 2pm. She comes back home at 4pm.
Personal History
Diet: Mixed
Appetite: Decreased due to pain
Sleep: adequate
Bowel and Bladder movements: Increased frequency of bowel movements, small quantities of stool.
No known allergies
Consumes Toddy in the summers
Menstrual history: She attained menopause 15 years ago.
Family History
No history of similar illnesses among immediate family members.
The patient is married and has one daughter (27yrs). Her husband died 25 years ago and she lost her son 10 years ago, both due to accidents.
No history of DM,HTN,CVA, TB, Asthma or CAD among her immediate family members.
General examination
The patient is conscious, coherent, co-operative; well oriented to time, place and person.
Moderately built, well nourished.
No pallor, icterus,cyanosis, clubbing, lymphadenopathy, edema.
Vitals
HR: 114 bpm
BP: 130/100 mmHg
RR: 20cpm
TEMP: 98.8
SpO2 at RA: 98%
GRBS: 98 mg%
Systemic Examination
RS: BAE+, NVBS
- Chest is symmetrical
- Trachea is central
- Chest expansion is symmetrical b/l
CVS: S1, S2 heard; no murmurs
P/A: soft, non tender at the time of the examination, no organomegaly or ascites
CNS: Higher mental function : intact
Cranial nerve functions : normal and intact
Motor system:
•Muscle Bulk: Normal on inspection and palpation on all 4 limbs, uniform and symmetrical on right and left sides
Muscle tone: Normal in both upper and lower limbs on both the right and left sides
•Muscle power: Symmetrical on right and left sides, normal
•Reflexes: Both superficial and deep reflexes present and normal
Sensory system: Normal
Investigations:
HIV 1/2 RAPID TEST: REACTIVE
STOOL FOR OCCULT BLOOD: POSITIVE
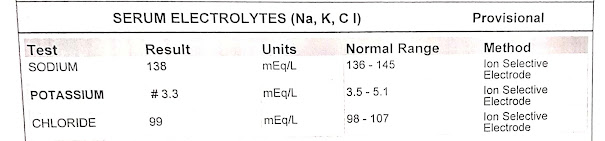
SERUM ELECTROLYTES: HYPOKALEMIA
SERUM CREATININE: ELEVATED
LFT: ELEVATED AST, ALT, ALP
HEMOGRAM: 12/6/22
BLOOD UREA
RANDOM BLOOD SUGAR
BLOOD GROUPING AND TYPING: O+
Provisional diagnosis: 60 year old female with HIV and gastroenteritis currently undergoing treatment.
Treatment:
- IV FLUIDS: 1 UNIT NS AND 1 UNIT RL AT 75ml/hr
- INJ CIPROFLOXACIN 500MG IV/ BD
- INJ ONDANSETRON 4MG IV/BD
- INJ PANTOPRAZOLE 40MG IV/OD
- CAP RACECADOTRIL 100MG PO BD
- INJ OPTINEURON( B COMPLEX) 1 AMP IN 100ML NS OD
- INJ METRONIDAZOLE 400MG IV/BD
- TAB SPOROLAC (PROBIOTIC)*2 PO TID
A 46 year old female who is a resident of Chintakunta and an agricultural labourer by occupation was brought to the casualty with chief complaints of sudden distension of abdomen and difficulty in breathing since 1 week.
History of presenting illness
2014: The patient started experiencing pain in both her knee joints along with restricted mobility. She says it was starting then that she couldn't sit from a standing position or stand from a sitting position with ease anymore.
2021: The patient was apparently asymptomatic 1 year back when she developed dyspepsia for which she was prescribed some PPIs which she started using on and off to treat her symptoms. The patient says she has developed an intolerance to spicy food this past year.
6th June,2022: i) The patient woke up in the morning and left to work as usual with no complaints, but at 6 in the evening, she started experiencing a sudden difficulty in breathing and had to sit down to recover. She said she felt like there was a huge weight on her chest that wasn't allowing her to breath in fully.
ii) She noted a distension in her epigastric and right hypochondriac region that was not present the day before. The swelling was not assosciated with pain.
iii) She also complained of severe bilateral knee pain that was apparently worsened during this period.
9th June.2022: She once again experienced a heart burn but this time it was not relieved by her regular medication.
10th June,2022: She was admitted to the hospital where she currently is.
12th June,2022: As of this day, the patient reports shortness of breath even at rest. Her knee pain is aggravated by walking and relieved by rest. Her abdominal swelling is assosciated with mild pain on the right side.
No history of cough, cold or fever
No H/o, loose stools , constipation, burning micturition
No chest pain, palpitations or PND .
No H/o headaches.
Past history:
- Patient has had bilateral knee pain and difficulty is standing up from sitting position since 5 years
- She is not a known case of Diabetes Mellitus,Hypertension, Asthma, CAD, hypothyroidism, TB, RA.
- No drug history.
- No history of other recent illnesses.
Surgical history:
The patient underwent a caeserian section during the birth of her second child and was tubectomized 16 years ago.
Daily routine:
The patient lives with her husband and son. She wakes up at 5 am everyday, cleans her house, prepares meals for her family and leaves to work at 9. She has lunch at 2pm. She returns home at 5pm and rests for half an hour before she starts with her household chores and preparation of dinner. She goes to bed at 10pm.
The patient spends many hours under direct sunlight and has handled chemicals and pesticides in the past without personal protective equipement. She wears slippers to work.
Personal History
Diet: Mixed
Appetite: Normal
Sleep: adequate
Bowel and Bladder movements: Regular
No known allergies
No known addictions, does not indulge in alcohol.
Menstrual history: Attained menopause last year (Has not had menstrual bleeding for 13 months)
Family History
No history of similar illnesses among immediate family members.
The patient is married and has one son and one daughter.
No history of DM,HTN,CVA, TB, Asthma or CAD among her immediate family members.
General examination
The patient is conscious, coherent, co-operative; well oriented to time, place and person.
Moderately built, well nourished.
No pallor, icterus,cyanosis, clubbing, lymphadenopathy, edema.
Bilateral non tender swelling around knee joints.

HR: 86 bpm
BP: 120/80 mmHg in both arms
RR: 20cpm
TEMP: 99°F
SpO2 at RA: 96%
Systemic Examination
RS: BAE+, NVBS
- The patient has grade 4 SOB (MMRC scale)
- Chest is symmetrical
- Trachea is central
- Chest expansion is symmetrical b/l
- Resonant on both sides
- No adventitious sounds heard
CVS: S1, S2 heard; no murmurs
P/A:
- Distended
- Palpable mass in the Epigastric region extending 5cm below the subcostal margin.
- No tenderness
- No fluid thrill or shifting dullness
- Normal Bowel sounds
- Liver is palpable.
Examination of the abdominal swelling:
- The swelling moves with respiration
- Cough impulse is positive
- There is no local rise of temperature
- Mild tenderness is present
CNS: Higher mental function : intact
Cranial nerve functions : normal and intact
Motor system:
•Muscle Bulk: Normal on inspection and palpation on all 4 limbs, uniform and symmetrical on right and left sides
Muscle tone: Normal in both upper and lower limbs on both the right and left sides
•Muscle power: Symmetrical on right and left sides, normal
upper limbs: 5/5
lower limbs: 5/5
•Reflexes: Both superficial and deep reflexes present and normal
No involuntary movements
Sensory system: Normal
Investigations:
8PM: 282 mg/dl
6AM: 257 mg/dl


COLOUR DOPPLER 2D-ECHO
- Sclerotic Aortic Valve
- Good LV systolic function
- Mild diastolic dysfunction (mild TR)
ULTRASOUND REPORT
- 15mm defect noted in the Epigastrium with herniated contents( Omentum included)
- Grade 2 fatty liver
Provisional diagnosis: 46 year old female with abdominal distension, acid peptic disease and denovo type 2 Diabetes Mellitus currently undergoing conservative treatment.
Treatment:
INJ NPH: 4U AT 8AM AND 4U AND 8PM
INJ HAI: 6U AT 8AM, 6U AT 2PM, 6U AT 8PM
INJ PANTOPRAZOLE 40MG IV OD
TAB PARACETAMOL+TRAMADOL PO (1/2 TABLET) SOS
INJ OPTINEURON( B COMPLEX) IN 100ML NS IV OD









































Comments
Post a Comment