Case:
A 65 year old male patient came to the opd with chief complaints of right sided weakness, deviation of mouth and drooling of saliva
History of present illness:
Patient was apparently asymptomatic 10days back then he developed weakness in right upper limb and lower limb, deviation of mouth, slurred speech and drooling of Saliva from mouth which is sudden in onset, progressive in nature .
It is not associated with difficulty in breathing, difficulty in lifting head off the pillow.
There is no history of trauma,headache, vomiting, diarrhoea,chest pain,calftenderness.
Pasthistory:
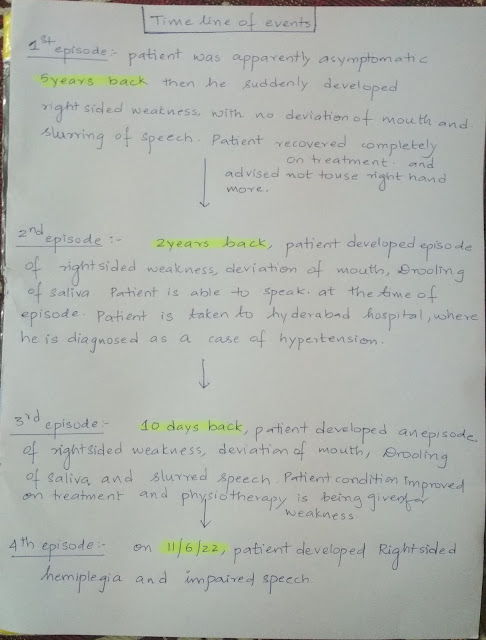
History of similar complaints in the past.
Patient is a known case of hypertension on medication.
Not a known case of DM, epilepsy,asthma.
Personal history:
Diet: stopped non veg 5years back
Appetite: normal
Bowel and bladder movements: normal
No significant weight loss
Occasional drinker
No allergies
Family history:not significant
General examination:
Patient is examined with an informed consent and well illuminated room
patient is well oriented to time but not to place and person
Moderately built and nourished
No pallor,icterus,cyanosis, clubbing,cyanosis lymphadenopathy, edema
Vitals:
Temperature:Afebrile
PR:70bpm
RR:16cpm
BP:140/80mm of hg
Systemic examination ;
CVS: s1 s2 heard
No murmurs
Respiratory system; normal vesicular breath sounds are heard
Abdomen: soft non tender no organomegly
CNS;
Higher functions:
Right handed
Conscious
Oriented to time not place and person
Memory: recent- present
Immediate: present
Remote: absent
Speech:
Not spontaneous
comprehension- present
Naming- absent
Repetition- absent
Disarticulation of speech - present
No delusions or hallucinations
Cranial nerve examination:
I- Olfactory nerve- sense of smell present
II- Optic nerve- direct and indirect light reflex present.
III-Oculomotor nerve, IV- Trochlear and VI- Abducens- no diplopia, nystagmus or ptosis
V- Trigeminal nerve- Masseter, temporalis and pterygoid muscles are normal. Corneal reflex is present.
VII- Facial nerve- face is symmetrical, unable to do forehead wrinkling, left nasolabial fold prominent than right.
VIII- Vestibulocochlear nerve- no hearing loss
IX- Glossopharyngeal nerve. X- Vagus- uvula not visualised
XI- Accessory nerve- sternocleidomastoid contraction present
XII- Hypoglossal nerve- Movements of tongue are normal, no fasciculations, no deviation of tongue
Spinomotor system:
Right Left
BULK: U/L- arm 24.5 cm 26 cm
-forearm 18 cm 18 cm
L/L- thigh 44 cm 44 cm
- leg 28 cm 28 cm
TONE: U/L decreased normal
L/L decreased normal
4c) Sensory system examination:
Right Left
crudetouch:. Absent present
fine touch : absent present
pain absent present
vibration absent present
temperature absent present
stereognosis- absent present
2 pt discrimination- absent present
graphaesthesia- absent present
Right Left
POWER: U/L- hand 0/5 5/5
- elbow 0/5 4/5
- shoulder 0/5 5/5
L/L- hip 0/5 4/5
- knee 0/5 5/5
- ankle 0/5 4/5
REFLEXES: Biceps +++ ++
Triceps +++ ++
Supinator +++ ++
Knee +++ ++
Ankle +++ ++
Plantar extension neutral
Reflexes of right upper limb and lower limb:
Tone of right upper limb and lower limb:
Babinski sign:
Investigation
CBP
Hemoglobin- 12.6 gm/dl (N)
PCV- 35.2 % (N)
TLC- 8600/ cumm (N)
RBC- 4.33 million/cumm (N)
Platelets- 2.58 lakhs/ml (N)
Blood urea- 24 mg/dl (N)
Serum creatinine- 1.3 mg/dl (N)
Serum sodium- 136 mEq/L (N)
Serum potassium- 3.7 mmol/l (N)
Serum chloride- 104 mEq/L (N)
LFT
Total bilirubin- 0.61 mg/dl (N)
Direct bilirubin- 0.16 mg/dl (N)
SGPT- 11 (N)
SGOT- 13 (N)
ALP- 105 IU/L (N)Albumin- 4 g/dl (N)

PROVISIONAL DIAGNOSIS:
Acute ischemic stroke causing right sided hemiplegia (left MCA territory)
Recurrent CVA
TREATMENT:
Tab. Ecosporine 150mg
Tab. Clopidogrel 75 mg
Tab. Atorvas 40mg
Tab. Atenolol 25mg
Physiotherapy
----------------------------------------------------------------------------------------------------------------------------------------
SHORT CASE:
A 52year old male patient came to the opd with Cheif complaints :
Fever since 4days
Abdominal distension since 3days
AbdominalPain since 3days
History of present illness:
Patient was apparently asymptomatic 4days back then he developed fever which is of low grade , continuous in Nature,not associated with chills and rigors,no aggravating factors, relieved on medication.
He then developed abdominal distension which is insidious in onset, progressive type associated with pain .
Before admission in our hospital he went to near by hospital where he diagnosed with thrombocytopenia.
No history of headache, vomiting, generalized body weakness
No history of loose stools, weight loss
Past history:
No similar complaints in the past
Not a known case of Diabetes mellitus,Hypertension, asthma,Epilepsy,cardiovascular disease.
Personal history :
Diet :mixed
Appetite:decreased
Bowel and bladder movements:normal
Sleep:adequate
Occasional drinker
No significant weight loss
No history of allergies.
Family history: nonsignificant
GENERAL EXAMINATION:
Patient is examined with an informed consent and in a well illuminated room
Patient is conscious, coherent and cooperative, well oriented to time, place and person
Moderately built and moderately nourished
No pallor, icterus, cyanosis, clubbing, koilonychia, lymphadenopathy
Vitals:
TEMPERATURE: afebrile
PR:84bpm
RR:22cpm
BP:110/70mmhg
Systemic examination:
CVS:
S1,S2 sounds heard,no murmurs
Respiratory system:
Bilateral vesicular breath sounds heard
CNS:
Higher mental functions are normal,sensory, motor and Cranial nerves are intact.
Abdominal examination:
Inspection:
Shape: distended
Flanks full dilated
Umbilicus: inverted
Skin is normal
no visible peristalsis
No visible pulsations
No scars and sinuses
Palpation:
No local rise of temperature
Tenderness-slightly
Liver-not palpable
Spleen: not palpable
No palpable mass
Percussion :
Dull note heard
Auscultation:
Provisional diagnosis:
Viral pyrexia with thrombocytopenia
INVESTIGATIONS-
Complete blood picture-
Hb-14.9g%
WBC-10,500 cells/mm3
Platelets-17000/mm3@outside hospital report
On 8/06/22:
Platelets-22000 /cumm
Neutrophils -43%
Lymphocytes -48 %
Eoisinophils -01%
Blood urea-59 mg/dl
Serum creatinine -1.6mg/dl
Serum electrolytes:
Na-142 mEq/l
K-3.9mEq/l
Cl-103 mEq/l
Liver function tests-
Total bilirubin-1.27 mg/dl
Direct bilirubin-0.44 mg/dl
SGOT-60 IU/L
SGPT-47IU/L
ALP-127IU/L
TOtal proteins- 5.9 gm/dl
Albumin-3.5g/dl
A/G ratio-1.48
COmplete urine examination-
Albumin -positive
Pus cells -4-5
Epithelial cells -2-3
NS1 ANTIGEN - POSITIVE
SEROLOGY -IgM and IgG negative
on 9/06/22-
Hb- 14.3g%
Platelets- 30,000/cumm
On 10/06/22-
Hb-14.0 g%
Platelets-84000/cumm
USG-
 IMPRESSION-
IMPRESSION-GRADE 2 FATTY LIVER
MILD SPLENOMEGALY
RIGHT SIDE PLEURAL EFFUSION (MILD)
MILD ASCITES
Fever chart
Treatment-
*On 8/6/22
IV FLUIDS - NS AND RL@100ML/hr
Inj.pan 40 mg iv /oD
Inj.optineuron 1 amp in 100 ml Na iv/OD over 30 mins
Inj.zofer 4 mg iv/SOS
VITALS monitoring 4th hourly
*On 9/6/22
Iv fluids - Ns/RL @100 ml/hr
Inj.pan 40 mg iv/OD
Inj.optineuron 1 amp in 100 ml/Ns/iv/OD over 30 mins
Inj.zofer 4mg/iv/sos
Tab.doxycycline 100mg PO/BD
VITALS monitoring
*On 10/06/22;
Iv fluids - NS,RL@100 ml/hr
Inj.pan 40 mg iv/oD
Tab.doxycycline 100 mg Po/BD
Inj zofer 1 amp iv/sos
Inj.optineuron 1 amp in 100 ml Ns/iv/OD over 30 mins
VITALS monitoring 4 th hourly
*On 11/06/22-
Iv fluids - NS,RL@100 ml/hr
Inj.pan 40 mg iv/oD
Tab.doxycycline 100 mg Po/BD
Inj zofer 1 amp iv/sos
Inj.optineuron 1 amp in 100 ml Ns/iv/OD over 30 mins
DOLO 650mg /sos
VITALS monitoring














Comments
Post a Comment