1701006177 CASE PRESENTATION
LONG CASE:
22 year old female housewife resident of Nalgonda district came to OPD on 10th June 2022
With the chief complaints of
* generalized swelling of body since 5 days
* reduced urine output since 5 days
* shortness of breath since 5 days
HISTORY OF PRESENTING ILLNESS
Paitent was apparently asymptomatic 5 days ago then she had developed generalized swelling and reduced urine output
No complaints of palpitations, cold, cough, burning micturition fever,chest pain,
PAST HISTORY
In 2010 when Paitent was 10 years old marked
*increased appetite
* increased urine output
*increased thirst
Were noted and she was taken to a local hospital where she was diagnosed with DIABETES and is on insulin therapy from then
In 2021
When she went to a regular check up she was diagnosed with hypertension from then she is on regular medication
* tablet Telma 40mg
*tablet Nicardia 20 mg
In May 2022
When she was 22 years old she had developed
*facial puffiness
*odema in feet
* shortness of breath
Grade IV
Where she was treated with dialysis and was send home
JUNE 2022(Presently)
after 15days of dialysis treatment Paitent had again developed
*generalized oedema
* reduced urine output
* loss of appetite
* vomiting
Paitent is a know case of
*diabetes melittus since past 12 years
*hypertension since 1 year
Not a know case of asthma epilepsy tuberculosis
PERSONAL HISTORY
appetite - reduced since 15 days
Diet - mixed
Bladder movements - reduced
Bowel movements - reduced
allergy - Not known
Addiction - NIL
ON EXAMINATION
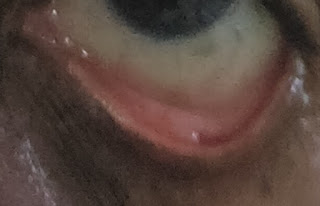
Pallor present
NO
icterus
cyanosis
clubbing
lymphadenopathy
oedema present
VITALS
ON 14TH
PR 86 bpm
BP 180/100mm hg
RR 24 cpm
Spo2 97%
SYSTEMIC EXAMINATION
CVS: S1 S2 heard
No murmur heard
RS: bilateral crepitus heard
CNS: Crainial Nevers intact
Motor system intact
Sensory pain temp touch vibration well appreciated
Per Abdominal :
Inspection: distendent
Flanks full
Umbilicus center.
Palpation : soft and non tender
No organomegaly
Percussion fluid thrill present
DAIGONOSIS
CKD ON MHD
TREATMENT
Injection
PIPTAZ 2.25gm /TID/IV
PAN IV/BD
ZOFER IV/TID
Lasix 60 mg /BD
tablet
NICARDIA 20 MG /BD
TELMA 40 MG /OD
OROFER-X5 PO/OD
NODOSIS 500 MG PO/BD
SHELCAL 500MG/PO/OD
-------------------------------------------------------
SHORT CASE:
A 52 year old male who is a toddy collector by occupation and resident of Nalgonda came to OPD on 8/6/22 with the chief complaints of fever since 4 days,
decreased appetite since 3days,
tightness of abdomen since 3days.
History of present illness:
-Patient was apparently asymptomatic 4 days ago. He then developed fever of low grade, sudden in onset, gradually progressive and relieved on medication.
-He also had complaints of abdominal distension which was gradual and progressive in nature. It is associated with pain. Abdominal pain aggravated on intake of liquids, solids.
- abdominal tightness is also present.
-Patient then approached local RMP and was given medication for 4 days. But symptoms recurred the next day.
No history of rashes ,bleeding tendencies
No history of headache ,vomitings, generalised body pains
No history of loose stools , pain abdomen
No history of weight loss
Past history-
Not a k/c/o DM ,HTN, TB,ASTHMA,cva, cad
Personal history :
Diet :mixed
Appetite : normal
Sleep : adequate
Bowel and bladder movements:regular
Occasional alcoholic & toddy intake
Family history :
Not significant
General examination:
Patient is consious, coherent, cooperative.
No signs of icterus, pallor,clubbing, lymphadenopathy, edema.
Vitals:
Temp: 98.6 F
PR: 84 bpm
RR: 20 cpm
Grbs: 115 mg/dl
Spo2: 98%
Systemic examination
Per Abdomen
Inspection:
Skin - smooth (scar from childhood)
Shape - distended
Umbilicus - normal
Abdominal wall movements - present
No visible pulsations and peristaltic movements seen.
Palpation:
Tenderness - mild
No rise of temperature
Liver - not palpable
Spleen - mild palpable
Gall bladder - not palpable
Kidneys - not palpable
Percussion:
Liver - dull note
Spleen - dull note
No shifting dullness, fluid thrill.
Auscultation:
Bowel sounds heard.
No bruit.
CARDIOVASCULAR SYSTEM-
Inspection-
The chest wall is bilaterally symmetrical.
No dilated veins, scars or sinuses are seen
Apical impulse or pulsations can be appreciated in sixth intercostal space 2cms lateral to mid clavicular line
Palpation-
Apical impulse is felt in the sixth intercostal space, 2 cm away from the midclavicular line
No parasternal heave or thrills are felt
Percussion-
Right and left borders of the heart are percussed
Auscultation-
S1 and S2 heard, no added thrills and murmurs are heard
RESPIRATORY SYSTEM-
Inspection-
Chest is bilaterally symmetrical
The trachea is positioned centrally
Apical impulse is not appreciated
Chest moves normally with respiration
No dilated veins, scars or sinuses are seen
Palpation-
Trachea is felt in the midline
Chest moves equally on both sides
Apical impulse is felt in the sixth intercostal space
Tactile vocal fremitus- appreciated
Percussion-
The areas percussed include the supraclavicular, infraclavicular, mammary, axillary, infraaxillary, suprascapular, infrascapular areas.
They are all resonant.
Auscultation-
Normal vesicular breath sounds are heard
Central nervous system:
No abnormalities detected
INVESTIGATIONS
Hemogram:
Hb-14.9
TLC-10,500
N-43
L-48
E-01
RBC-5.02
PLT-22,000
Blood urea-59
Serum creatinine-1.6
Serum Electrolytes-
Na+ :141
K+ :3.9
Cl- :103
LFT
Total bilirubin -1.27
Direct bilirubin -0.44
SGOT-60
SGPT-47
ALP-127
Total protein-5.9
Albumin-3.5
A/G ratio-1.48
CUE
ALbumin- ++
Pus cells -4.6
Epithelial cells:2-3
USG :
Fatty liver (grade 2)
Mild splenomegaly
Mild pleural effusion in right lungs
Provisional diagnosis:
-viral pyrexia with thrombocytopenia
O/E :
Pt is conscious,coherent ,cooperative
Temp: 103 F
Bp: 120/ 70mmhg
Pr: 90 bpm
RR: 24 cpm
SYSTEMIC EXAMINATION:
CVS:
S1, S2 heard. No murmurs heard.
RS:
Bilateral air entry present
Per abdomen:
Soft, mild tenderness
Shape: distended
Bowel sounds heard.
Treatment
On 13th
Oral fluids
Tab dolo 650 mg/po/sos
Tab pan 40 mg
Doxycycline 100 mg
Zincovit
8th hourly monitoring of vitals













Comments
Post a Comment