1701006146 CASE PRESENTATION
Long case
Presenting compalaints
13year old female
Came with chief complaints of Shortness of breath since yesterday
4 episodes of vomitings since yesterday 10pm
Birth history
1st child
2nd degree consanguineous marriage
Born in 2010
LSCS
Father has no idea about immunisation status
Mother-has 2 children
The current pt is the elder one(birth in 2010)
2nd child born in 2013
In 2014 mother diagnosed with kochs-expired in 2022 sept(did not use ATT regularly)
History of presenting illness
Patient was apparently asymptotic till the age of 11years
She was sent to hostel for studies
After few days of hostel stay she noticed that she has bilateral neck swellings
So she was taken to RMP with complaints of neck swellings,fever and cough on and off
RMP has initiated her on ATT as her mother has also has kochs
They used ATT for 2months started in 2021 june
After initiating ATT fever increased so they stopped ATT and was referred to Hyd by the RMP
Patient was taken to NF hospital where she was evaluated for kochs but none of the investigations showed AFB,at that time she also had complaints of knee pains and wrist joint pains
In view of joint pains she was referred to N hospital
In N hospital they suspected it to be autoimmune and started her on Tab Wysolone and Tab HCQ ,which she used for 15 days and stopped and later did not go there for follow up
(ANA ELISA-equivocal,ANA IFA-negative,Anti Ds DNA ELISA-Positive,Anti Ds DNA IFA negative)
She was taken to another local hospital with c/o joint pains,facial puffiness,pedal edema,fever ,cough
Lymph node biopsy was done in May 2022 ?reactive(no report available but attendor was informed that it was negative for kochs)
So Mycobacterial gene expert test was done on blood sample which was also negative
But she was initiated on ATT empirically on may/2022.
10-15days before starting ATT attendors have noticed that she is developing facial rash and Hair loss,due to hair loss scalp rash also became evident.
History of past illness:
K/C/o extra pulmonary tb (1year back used att for 6 months)
N/k/c/o hypertension, DM, epilepsy, cad, Cva
Treatment history:
Used att for 6 months for extra pulmonary tb.
Personal history:
Single
Occupation:student
Decreased appetite and micturition
General examination:
Pallor +
Edema +
No icterus cyanosis clubbing lymphadenopathy
Systemic examination:
CVS: s1 s2 heard, no murmurs
RS: BAE + , NVBS
P/a : free fluid present
Tenderness + at right and left hypochondria and epigastrium
Cns: pt is C/C/C
No FND
HMF +
Right. Left
Biceps. ++ ++
Triceps. 2+ 2+
Supinator. + +
Knee 2+ 2+
Ankle. + +
Clinical images

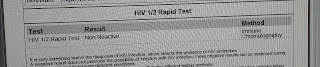
Investigations
Differential Diagnosis
Glomerulonephritis secondary to ? Lupus ? Autoimmune etiology with polyserositis secondary to autoimmune / ? Tuberculosis
Treatment
1. FLUID RESTRICTION LESS THAN 1.5L/DAY
2. SALT RESTRICTION LESS THAN 1.2GM/DAY
3. INJ. LASIX 40 MG IV/BD
4. INJ. MONOCEF 1GM IV/BD(D2)
5. INJ. METHYLPREDNISOLONE 250 MG IN 100ML NS IV/OD
6. TAB. ALDACTONE 25MG PO/OD
7. TAB. SHELCAL 500 MG PO/OD
8. VITALS MONITORING
--------------------------------------------------------------------------------------------------------------------------
short case
40year old male who is a farmer by occupation and came to opd with
CHIEF COMPLAINTS;
loose stools yesterday 2 a.m
vomiting since today morning
HISTORY OF PRESENT ILLNESS;
Patient was apparently asymptomatic till yesterday evening then
he suddenly developed loose stools yesterday night @ 2 a.m 40 to 50 episodes of loose stools,large quantity, white coloured stools,foul smelling, non blood tinged
c/o vomiting 3 episodes in the morning, food particles as content,non projectile, non bilious, non foul smelling relieved on their own.for loose stools they went to local RMP and got symptomatic treatment
similar episodes of vomiting and loose stools 10 years back and got admitted for 1 week and discharged
H/O insecticides spray yesterday morning
No H/O outside food and water intake .No similar complaints to his family,neighbours
No h/o fever,cough,cold
PAST HISTORY;
N/k/c/o DM,HTN,TB,EPILEPSY, CVA,CAD,THYROID DISORDERS
FAMILY HISTORY:-
Insignificant
PERSONAL HISTORY:-
DIET-mixed
APEPTITE- decreased
BOWEL &BLADDER-Increased,increased burning micturition since today
SLEEP-Adequate.
ADDICTIONS- No
GENERAL EXAMINATION:-
Patient is conscious , coherent,cooperative.
Well oriented to time place & person
Moderate built and moderately nourished.
Pallor absent
No cyanosis, clubbing, icterus, LN
Vitals :
Bp -140/100 mmhg
PR -96 bpm ;
RR : 22cpm
Spo2 : 96 on RA
GRBS:128 mg/dl
CENTRAL NERVOUS SYSTEM;
patient is conscious
speech is normal
no signs of meningeal irritation
Sensory examination: Normal
reflexes;
RIGHT LEFT
BICEPS +2 +2
TRICEPS +2 +2
SUPINATOR +1 +1
KNEE +2 +2
ANKLE +2 +2
Rhomberg's negative
Cerebellum:
Nystagmus-absent
Tremors- absent
Finger nose test- normal
Dysdiadokinesia- absent
CARDIOVASCULAR SYSTEM:-
S1 S2 heard
No murmurs.
RESPIRATORY SYSTEM:-
Dyspnea-absent
No wheeze
Breath sounds - vesicular
No Adventitious sounds
ABDOMINAL EXAMINATION:-
No tenderness
No palpable liver and spleen.
Bowel sounds - PRESENT
INVESTIGATIONS;
USG
2D-ECHO
PROVISIONAL DIAGNOSIS: Acutw gastroenteritis secondary to ?vibrio cholera with non oliguric aki
TREATMENT
1.IVF 2NS.1DNS.2RL@100 ml/hr
2. Inj.metrogyl 100 ml I.V TID
3.Inj.pan 40 mg I.V OD(BEFORE breakfast)
4.Inj.zofer 10 mg I V sos
5.Inj.Neomal 1 gm I.V sos
6.Tab.dolo 650 mg PO SOS
7.Tab.Redtoil 100 mg Po/TID
8.Tab.sporolac-DS PO/TID
9.ORS in glass of water /SIPS WITH EACH EPISODES
10.Tab.OFLOX 300 mg PO/BD
11.BP.PR.RR.TEMP charting 4th hourly





































Comments
Post a Comment