1801006021 CASE PRESENTATION
Long case
A 29 year old female know case of SLE , customer service executor by occupation, resident of akkinepalli came to OPD with cheif complaints of swelling of both legs and swelling around eyes since 3 days .
*History of presenting illness:-
Pateint was apparently asymptomatic 6 years back then she developed oral ulcers and rash on face and joint pains , hair loss without scaring due to which she went to a hospital and diagnosed with sle (2017).
She was on hcq 200 ,wysolone,azr medication continuously till November 2022
In November she was admitted to kims emergency due shortness of breath which is sudden in onset gradually progressed ,they diagnosed it as kidney failure and did dialysis four times and sent her home with some medication.she was also diagnosed with hypertension and started on nicardia 30 mg .
But after 2 months on February 5 th she was admitted to hospital with history of vomitings and diarrhea since 10 days and diagnosed as acute kidney injury on chronic renal failure, they started her on dialysis and given below medication
Rabeprazole + domperidone
Tab orofer xt po/od 8am
Tab shelcal 500mg po/od
Tab sodium bicarbonate 500mg po/bd
Tab nicardia 20mg po/tid
Probiotics
Since then she is coming to hospital for regular dialysis that is once in 3 days .
H/o edema of legs upto knees since 3 days , pitting type which is insidious in onset gradually progressive.
H/o reduced urine output
H/o puffiness around the eyes since 3 days ,prominent during morning and subsides by night
*Past history :-
Diagnosed with hypertension 5 months back ( on November 2022 secondary to kidney failure) and on regular medication.
Not a known case of diabetes mellitus, tuberculosis, thyroid disorders, epilepsy
*Personal history:-
daily routine her day starts at 7 AM ,she used to get ready for work and went to office at 8 AM ,used have breakfast at office at around 10 am ,her work was more of attending client calls with 1 to 2 breaks in between till 6 PM more of sedentary work ,sleeps at 11 pm .But since one month she is staying in home ,she quit her job due to regular dialysis.
Diet - mixed
Appatite- loss of appetite
Sleep- adequate
Bowel and bladder - bowel regular, reduced urine output
No Addictions
*Family history:-
Mother is known diabetic
No history of autoimmune diseases in the family.
MENSTRUAL HISTROY:
Age of menarche:12 years.
Menstrual cycles :Her Menstrual cycles were irregular since 2 months.
Her last Menstrual period was Dec 25th 2022
Obstetric history:- para 2 live 1
*General examination:-
Patient is conscious, coherent, cooperative
Well oriented to time place and person,moderately nourished thin built.
Pallor:- present
Icterus, cyanosis, clubbing, generalized lymphadenopathy are absent
Bilateral pedam edema present, pitting type
*Systemic examination:-
CVS:
S1 ,S2 present
No murmurs
Respiratory system:
Bilateral air entry present
Normal vesicular breath sounds heard
No dyspnoea and no wheeze
Per abdomen:
Shape of abdomen:
scaphoid
Liver and spleen are not palpable
CNS:
Patient is conscious
Speech: normal
Cranial nerves: normal
Motor and sensory system: normal
Glassgow coma scale: E4 V5 M6
*INVESTIGATIONS:
15.03.2023
Blood urea -79 mg/dl (N=12 to 42 mg/dl)
Serum creatinine-4mg/dl(N0.6 to 1.1)
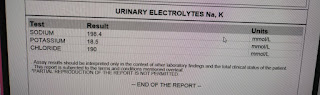
Serum electrolytes-
Na :141mEq/L(N-136 to 145)
K:3.5mEq/L(N:3.5 to 5.1)
Cl:102mEq/L(N=98 to 107)
Ionized ca+2:1.01mmol/L.
14.02.2023
HEMOGRAM:
Hb 8.5gm/dl.
Total count:12000 cell /cumm
Neutrophils:83 %
Lymphocytes:11%
Pcv:24.3 volume %
Platelets :l.lL / cumm.
Impression :Normocytic normochromic anemia with neutrophilic lymphocytes and thrombocytopenia.
Renal function test:
Urea:157mg/dl
Creatinine :6.9 mg/dl.
Uric acid :6.5 mg/dl.
ECG:-
**Provisional diagnosis:-
Chronic renal failure secondary to lupus nephritis on maintaining hemodialysis.
*Treatment:
Tab Nicradia 30mg,po/tid
Tab lasix 40mg , po/bd .
Tab wysolone,po/bd.
Tab azathioprine 50 mg po/ od
Tab hydroxychloroquine 200mg po/od.
Tab Met xL 25 mg ,po/od.
Tab nodosis 500mg po/od.
Tablet shelcal 500mg po/od
Tab orofer xt po/od
Tab Pan 40mg po/od.
Tab blod3 po/ weekly twice .
----------------------------------------------------------------------------------------------------------------------------------------------------
short case
35 YR OlD MALE PATIENT , LORRY DRIVER BY OCCUPATION , RESIDENT OF ATTHAMPET ,CAME TO THE OPD WITH THE
C/O Pain abdomen since 10days,
yellowish discolouration of urine since 8 days
Distension of abdomen since 6 days
Bilateral lower limb swelling since 5 days .
HISTORY OF PRESENTING ILLNESS :
Patient was apparently asymptomatic 10days ago and then developed,abdominal pain ,which was insidious in onset and gradually progressive ,which was of dragging type and diffuse, No aggravating factors but relieved on medication and reccured on stoping medication ,but not relieved on leaning forward .
Yellowish discolouration of urine since 8 days, NOT ASSOCIATED with any poor stream ,pyuria ,hematuria ,increased frequency , nocturia ,Burning micturition but decreased urine output present since 5days
Abdominal distension
and bilateral lower limbs edema since 6days,which were insidious in onset and gradually progressive, pitting type of edema over bilateral lower limbs,till knees
Pitting Type Of Edema :
Constipation since 5 days, Not associatied with passage of blood in stool /melena
PAST HISTORY:
No history of similar complaints in the past
K/C/O DIABETES MELLITUS ,which was diagnosed 5 months ago and started on ORAL HYPOGLYCEMIC DRUGS ( pt couldnt remember the drugs names )
N/K/C/O HTN , EPILEPSY ,CAD,CVA ,TB ,ASTHMA
PERSONAL HISTORY:
Sleep - Disturbed since 10days.
Diet - Mixed
Appetite - Disturbed since 6 days
Bowel and bladder movements : IRREGULAR ( decreased urine output and Stools not passed since 5 days )
Addictions : Alcoholic and chronic smoker since 10years
GENERAL EXAMINATION:
Patient is drowsy not coherent and not co operative, moderately built and nourished.
Vitals at presentation
Temp : Afebrile
BP: 110/80mmHg
PR: 86bpm
RR: 20cpm
SpO2 : 98%
Pallor - absent
Icterus - present -
Cyanosis:- absent
Clubbing - absent
Lymphadenopathy : absent
Edema : Present till knee level and of pitting type
PER ABDOMEN
Patient was examined after taking consent in a well lit room
ON INSPECTION
Abdomen is distended
umbilicus is inverted
Skin over abdomen is stretched and shiny
No visible pulsations
Engorged veins - Present
PALPATION :
all inspectory findings confirmed
No rise of temperature and tenderness
No guarding and rigidity
No hepatomegaly and Splenomegaly
PERCUSSION :
Shifting dullness - Present
Fluid thrills - Present
Puddle sign cannot be elicited ,as pt is not cooperative
AUSCULTATION :
Sluggish bowel sounds are heard
No bruits
CVS : S1 and S2 heard
no murmurs
CNS: No flapping tremors( Asterexis )
(Apraxia cannot be elicited as pt is not cooperative )
Apraxia Charting after 5 days of Hospital Stay :
RS : bilateral air entry is present
INVESTIGATIONS:
ASCITIC TAP DONE and fluid sent for analysis :
ASCITIC TAP DONE and fluid sent for analysis :
ABG :
CT scan : Showing Calcifications:
CT scan : Showing Calcifications:
Chest Xray:USG REPORT:
Enlarged liver with altered echotexture s/o CLD
gall bladder edema with sludge
Gross ascitis
Provisional Diagnosis :
Chronic liver disease 2° to alcohol intake with Type II DM
Alcohol dependence Syndrome
Chronic pancreatitis
MANAGEMENT:
) IV fluid NS 50 ml /hr
2) inj lasix 40mg IV /BD
3) T. Aldactone 50mg RT /OD
5) Syp . Lactulose 15ml RT /TID
6) Salt and fluid restriction ; Salt < 2gm /day , fluid < 1.5 lit /day
7) inj 3 amp KCL in 500ml NS over 5 hrs
8) Weight and abdominal girth daily
9) GRBS monitoring 2nd hrly
10) vitals monitoring 4th hrly
12) inj .Thiamine 200mg IV /BD
13) 3-4 egg whites /day
14) protein X powder 3-4 scoops in glass of milk RT/TID.
Follow up:-
Patient visited two times since December
Maintenance on
*Udiliv- 300
*Viboliv
*Thiamine
Abdominal distention and jaundice subsided.
















































Comments
Post a Comment