1801006030 CASE PRESENTATION
LONG CASE
CHIEF COMPLAINTS:-
27 yr old male patient came to our hospital to seek medical advise for removal of tracheostomy tube.
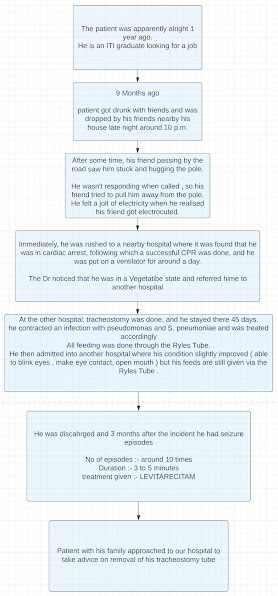
HISTORY OF PRESENTING ILLNESS : -
PSYCHOLOGICAL HISTORY:-
When young, patient was a good kid and enthusiastic.
When he was 6 yrs old he lost his father (who was a heavy drinker and was a daily wage labourer ).
After this event his mother become the sole bread winner of the family.
His brother left the house for further education, during this time the patient started to make friends then he got addicted to alcohol.
He wasn't great with studies and used to roam jobless, he started coming to home later night.
He on his mother's request completed graduation and then started to look for a job, to support the family.
PAST HISTORY: -
● He had several episodes of seizures 3 months later following the electric shock.
● Not a known case of HTN, DM , Asthma , TB
● Tracheostomy was done.
FAMILY HISTORY:-
● Father passed away and he was a heavy drinker
● Mother :- Not a known car of HTM, DM.
Mild knee pain in both lower limbs
. while climbing stairs
● Elder Brother :- Healthy
● Sister :- Healthy
PERSONAL HISTORY:-
Height :- 5'6 --> 164.67 cms
Weight :- 40 kg approx.
Appetite :- decreased
Diet :- feeding done through Ryle's Tube
Breakfast :- Protein powder shake
Afternoon:- Rice and dal with water
Snacks:- Biscuits and milk
Dinner :- Rice and dal with water
Sleep - Adequate
Bowel and Bladder movements- regular
ADDICTIONS : -
After his brother left for his further studies, patient got new friends and new habits with it at a young age.
● Alcohol - he started when he was around 16-17 yrs old.
Quantity unknown.
● Smoking - occasionally with friends.
● Tobacco chewing - Regular. Quantity is unknown.
TREATMENT HISTORY:-
Suction every 2 hourly.
Change in position every 2 hours.
Vitals monitoring every 4 hrs.
Tab RANITIDINE 150 mg PO/OD (morning before food)
T. LEVITARECITAM 500mg PO/OD (Night time)
T. SUPRA CAL [ CALCIUM CITRATE+VITAMIN K2-7+ CALCITRIOL ]PO/OD (after lunch)
GENERAL PHYSICAL EXAMINATION :-
Patient is in a vegetative state, uncooperative, appears thin, weak and malnourished
Pallor-absent
Icterus-absent
Cyanosis-absent
Clubbing-absent
Lymphadenopathy-absent
Pedal edema- absent
Koilonychia- absent
VITALS:-
Temperature- 2 pm -> 98.4°F
4 pm -> 98.6°F
6 pm -> 98.2°F
Pulse rate- 2 pm -> 102 bpm
4 pm -> 102 bpm
6 pm -> 100 bpm
Respiratory rate- 2 pm -> 26 cpm
4 pm -> 26 cpm
6 pm -> 18 cpm
BP - 2 pm, 4 pm, 6 pm -> 110/80 mm Hg
SpO² - 2 pm , 4 pm -> 98%
6 pm -> 100%
SYSTEMIC EXAMINATION:-
CENTRAL NERVOUS SYSTEM-
● GCS :- E4 V2 M4 At the time of examination
● Higher mental functions -
vegetative state, disoriented
Speech, memory and intellect couldn't be assessed.
Release Reflexes :-
Grasp reflex :- couldn't be performed as patient kept his fists clenched.
Glabellar reflex :- absent
Pout Reflex :- absent
Palmo-mental reflex :- couldn't be performed as patient kept his fists clenched.
● Cranial Nerve examination:-
pupillary reflex :Direct and indirect light reflex seen
Trigeminal:
Corneal and conjunctival present
Gag reflex is present
Tongue moments present
● Motor System :-
Right Left
UL LL UL LL
Bulk wasted wasted wasted wasted
Tone hypertonia normal hypertonia normal
Power :- 3/5 3/5 3/5 3/5
Reflexes :-
Biceps, Triceps, Supinator reflexes are absent
Knee reflex positive in both limbs
Ankle reflex positive in both limbs
Plantar reflex positive in both limbs
● Sensory System :- couldn't be elicited
● Myoclonic jerks are seen regularly
● Gait:- couldn't be elicited
CARDIOVASCULAR SYSTEM :-
S1 and S2 are heard.
No murmurs are heard
Apex beat felt at 5th ICS
RESPIRATORY SYSTEM :-
B/L basal crepitations are heard
ABDOMINAL SYSTEM:-
Soft and non tender
ENT EXAMINATION:-
Nose :-
External frame work is normal.
DNS to left is noticed.
Ryle's tube in the right nasal cavity.
Oral cavity and Oropharynx:
Couldnot be examined as patient is not co-operative.
Trachea:-
Central
Tracheostomy tube was placed
INVESTIGATIONS:-
X- RAY of neck :-
PROVISIONAL DIAGNOSIS :-
Hypoxic Ischemic Brain Injury Post CPR state
TREATMENT PLAN:-
After Neurology consultation , The Neurologist suggested for Family Counselling and Palliative Therapy.
References :-
Role of neuro rehabilitation in electrical injuries
https://pubmed.ncbi.nlm.nih.gov/8848659/
Use of vitamin k2 7 (Menaquinone) in hypoxic brain injury
https://pubmed.ncbi.nlm.nih.gov/33090426/
----------------------------------------------------------------------------------------------------------------
short case
43 year old male, daily wage worker by occupation came to medicine opd with complaints of
CHIEF COMPLAINTS :-
1) Abdominal pain since 5 days
2) Decreased urine output since 5 days
3) Vomiting since 4 days
4) Constipation since 4days
HISTORY OF PRESENTING ILLNESS:-
Patient was absolutely alright 5 days back then developed abdominal pain which was sudden in onset,diffuse in nature, sharp and continous with no aggrevating and relieving factors and associated with vomiting (4 episodes) which are non projectile and greenish in color
He also hasn't passed stools since 4 days and complained about decresed urine output since 5 days
There is a history of chronic alcoholism
-- He consumes alcohol daily ( approx 750 ml )
-- type whatever he finds cheap depending on his daily earnings.
He hadn't eating properly since last 10 days all he'd take was alcohol.
PAST HISTORY:
N/k/c/o DM, HTN, ASTHMA, TB, EPILEPSY
No history of previous surgeries.
FAMILY HISTORY :
No relevant family history
PERSONAL HISTORY:
Diet :- mixed
Appetite:- decreased since 10 days
Sleep :- disturbed and reduced
Smoking:- no
Gutka and khaini :- since 15 years
Alcohol :- He started consumption of alcohol twenty years ago (500ml) [ then he got married ]---> his wife expired ---> increased his alcohol consumption ( 750 ml/daily) --->his elder daughter also passed away 4 years back---> his alcohol consumption worsened since then
TREATMENT HISTORY :-
No relevant treatment history is available
GENERAL EXAMINATION :-
Patient is concious, coherent and cooperative
built:- malnourished
CAGE CRITERIA:- 4
Signs of dehydration are seen
- sunken eyes
-increased feeling of thirst
- dried lips and tongue
- skin pinch test more than 3 secs
GCS = 15
Pallor, , cyanosis, clubbing, lymphadenopathy are absent
Icterus is seen
VITALS :-
- Temp :- afebrile
- BP:- 100/70 mm Hg
FEVER CHARTING- RR :- 17 cpm
- PR :- 84 bpm
- SpO2 :- 99% on RA
SYSTEMIC EXAMINATION:-
CVS :- S1 S2 heard and no murmurs heard
RS :- BAE+ , NVBS , trcheal position is central
CNS :- HMF are functional and no focal neurological deficits are noticed.
P/A :- shape of abdomen is scaphoid
No flank fullness is seen
Umbilicus is inverted and no engorged veins
Hernial surfaces are normal
rigid and guarding is seen.
On palpation diffuse tenderness is seen
liver span :- 15 cm
No other organomegalies is felt.
bowel sounds were reduced [ 4/min ]INVESTIGATIONS :-
HEMOGRAM
HB 11.4GM/DL
TLC #23,200
N/L/E/M/B. #85/07/#00/08/00
PCV #31.8
MCV 88.6
MCH 31.8
MCHC 35.8
RDW-CV #14.5
RDW-SD #47.7
RBC. #3.59
PLT. 62,000
CUE :-
ALBUMIN ++
BILE SALTS AND PIGMENTS NIL
PUS CELLS NIL
LFT :-
Total Bilirubin #14MG/DL
Direct Bilirubin #13.20MG/DL
SGOT #94 IU/L
SGPT #50 IU/L
ALP. # 224 IU/L
TP # 4.9gm/dl
albumin. #2.4gm/dl
A/G RATIO. 0.96
RFT:
Blood urea #196 (6 to 24 mg/dL)
Serum creatinine #4.50.74 to (0.74 to 1.35 mg/dL)
Serum electrolytes
Sodium #119
Potassium #2.6
Chloride #94
Calcium #0.91
ABG:
PH 7.31
Pco2:#18.1
Po2:109
Hco3:#8.9
Blood group:A+ve
APTT 35sec
PT:18sec
INR:1.33
ESR:0.5mm/1st hour
LDH #469
serum amylase 1349 IU/L ( on 29th dec 2022 )Serum osmolality:265.4mosm/kg
Urinary electrolytes:
Sodium 169
Potassium 15
Chloride 180
ECG:-
2D-ECHO:-
DIAGNOSIS:-
Systemic Inflammatory Response Syndrome(acute pancreatitis?) a/w Multi Organ Dysfunction Syndrome
Dilated Cardio MyoPathy ( SIRS/ ALCOHOL INDUCED)
HYPONATREMIA
HYPOKALEMIA
Acute Kidney Injury
ACUTE LIVER INJURY ( ALCOHOL INDUCED )
?LEPTOSPIROSIS
TREATMENT:-
Inj. MEROPENEM 1gm iv stat F/b 500mg iv/BD
Inj. DOXY 100mg iv/BD
Inj. PAN. 40mg iv/OD
Inj. ZOFER 4mg iv/sos
Inj. NEOMOL 1gm iv/sis (if temp>101°f)
Inj. LASIX 40mg iv/BD
inj. OPTINEURON 1amp in 100ml NS iv/OD
Tab. UDILIV 300mg BD
SYP. HEPAMERZ 10ml TID
SYP. LACTULOSE 15ml HS
Inj. THIAMINE 200mg in 100ml NS.







.jpg)




.jpeg)
.jpeg)



Comments
Post a Comment