1801006076 CASE PRESENTATION
LONG CASE
A 29 year old female know case of SLE , customer service executor by occupation, resident of akkinepalli.
CHEIF COMPLAINTS :
- Swelling Of Both Legs Since 3 days
- Swelling Of Both Eyes Since 3 days
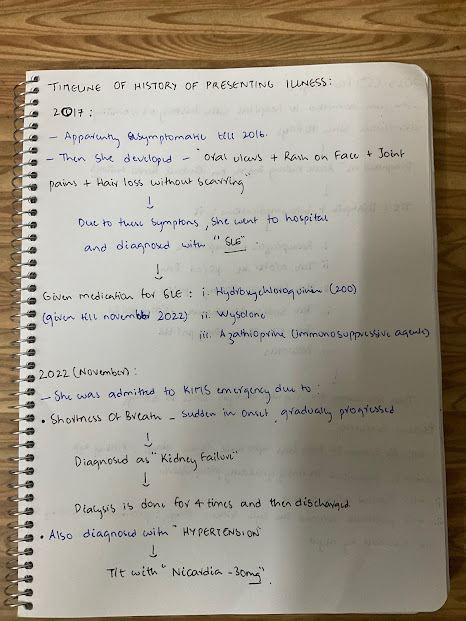
HISTORY OF PRESENTING ILLNESS :
Diagnosed with hypertension 5 months back ( on November 2022 secondary to kidney failure) and on regular medication.
Not a known case of diabetes mellitus, tuberculosis, thyroid disorders, epilepsy
PERSONAL HISTORY :
Her Daily routine day starts at 7 AM ,she used to get ready for work and went to office at 8 AM ,used have breakfast at office at around 10 am ,her work was more of attending client calls with 1 to 2 breaks in between till 6 PM more of sedentary work ,sleeps at 11 pm .But since one month she is staying in home ,she quit her job due to regular dialysis.
Diet - mixed
Appetite - loss of appetite
Sleep- adequate
Bowel and bladder - bowel regular, reduced urine output
No Addictions
FAMILY HISTORY :
Mother is known diabetic
No history of autoimmune diseases in the family.
MENSTRUAL HISTROY:
Age of menarche:12 years.
Menstrual cycles :Her Menstrual cycles were irregular since 2 months.
Her last Menstrual period was Dec 25th 2022
Obstetric history:- para 1live 1
GENERAL EXAMINATION :
Patient is conscious, coherent, cooperative
Well oriented to time place and person, moderately nourished thin built.
Pallor - Present
Icterus, cyanosis, clubbing, generalized lymphadenopathy are absent
Bilateral pedal edema present, pitting type
SYSTEMIC EXAMINATION :
CVS:
S1 ,S2 present
No murmurs
RESPIRATORY SYSTEM :
Bilateral air entry present
Normal vesicular breath sounds heard
No dyspnoea and no wheeze
ABDOMINAL EXAMINATION :
Shape of abdomen: scaphoid
Liver and spleen are not palpable
CNS:
Patient is conscious
Speech: normal
Cranial nerves: normal
Motor and sensory system: normal
Glassgow coma scale: E4 V5 M6
15.03.2023
Blood urea -79 mg/dl (N=12 to 42 mg/dl)
Serum creatinine-4mg/dl(N0.6 to 1.1)
Serum electrolytes-
Na :141mEq/L(N-136 to 145)
K:3.5mEq/L(N:3.5 to 5.1)
Cl:102mEq/L(N=98 to 107)
Ionized ca+2:1.01mmol/L.
14.02.2023
HEMOGRAM:
Hb 8.5gm/dl.
Total count:12000 cell /cumm
Neutrophils:83 %
Lymphocytes:11%
Pcv:24.3 volume %
Platelets :l.lL / cumm.
Impression :Normocytic normochromic anemia with neutrophilic lymphocytes and thrombocytopenia.
Renal function test:
Urea:157mg/dl
Creatinine :6.9 mg/dl.
Uric acid :6.5 mg/dl.
ECG:-
PROVISIONAL DIAGNOSIS :
Chronic renal failure secondary to lupus nephritis on maintaining hemodialysis.
TREATMENT :
Tab Nicardia 30mg,po/tid
Tab lasix 40mg , po/bd .
Tab wysolone,po/bd.
Tab azathioprine 50 mg po/ od
Tab hydroxychloroquine 200mg po/od.
Tab Met xL 25 mg ,po/od.
Tab nodosis 500mg po/od.
Tablet shelcal 500mg po/od
Tab orofer xt po/od
Tab Pan 40mg po/od.
Tab biod3 po/ weekly twice .

























Comments
Post a Comment