1801006077 CASE PRESENTATION
LONG CASE
A 13 year old female student from suryapet came to the OPD with chief complaints of
Vomitings on Monday night at 10 pm
breathlessness since 1 day
History of present illness:
Patient was apparently asymptomatic before 2020 that is till the age of 11 years,then she noticed swellings in the neck bilaterally,no pain, firm in consistency.
She also had fever which was insidious in onset , intermittent, no night rise of temperature, relieved with medication dolo 3 tid
She also had Non productive cough , no hemoptysis ,relieved with medication.
These symptoms was continued for 2-3 months.
After consulting rmp they started att as her mother has tuberculosis.
Eventually swellings size decreased and symptoms got relieved.
But the fever was not subsiding,so they stopped taking medication.
As rmp suggested , they went to hospital in Hyderabad and got her tested for tuberculosis:
-fnac
-cancer tests
- tb tests
-mantoux
-sputum culture
-cbnaat
because her mother is a known case of tuberculosis.
She got admitted for 10 days and recieved symptomatic treatment
She also had complaints of joint pains wrist and knee.
They suspected it to be automimmune and started her on Hcq and wysolone tab which they used for 15 days.
After that they tested for
ANA ELISA equivocal
ANA IFA negative
ANTI DS DNA ELISA positive
ANTI DS DNA IFA negative
So she went back home
2021
In June she started developing pigmentation/rash over face which then was seen on scalp evident because of hair loss and on trunk since 3 months,not associated with itching.
pedal edema which was upto ankles and progressed till knee in the last 3 months,pitting type.
Then she was taken to area hospital and got tested and the attender(father) was informed that she has tuberculosis.
2022
Ln biopsy was done in May
Mycobacterial gene expert test was done
No reports available
So they started her on ATT and recieved regular treatment for 6months.
2023
Her symptoms settled and she was fine until January 10 when she develop generalized edema.
They went to another hospital and got tested and was told to have proteinuria.
In January and February she had mild fever.
1 week back she developed fever and edema again.
On 13 March that is Monday night 10 pm she had episodes of vomiting 4 episodes ,food as contents,non bilious.
She also developed grade 2 sob and so they got her to here at 5.30am.
In 5th class her weight was 28kgs then in 6th class 23kgs,8th class 21 kgs
After att treatment her weight got improved to 23kgs that is last year
In December 26kgs, 24kgs ,yesterday it was 25kgs.
Past history
K/c/o tuberculosis
Not a known case of diabetes, hypertension, epilepsy, thyroid
Treatment history :
Used ATT for 6 months for TB
Personal history :
Single
Student
Daily routine:
She studied in local school until 4th class.
In 5th class she went to gurukul school and joined in hostel and was fine until 6th class.
In hostel
5 am wake up
Gets ready by 6 am
6:30 am to the ground for yoga,exercises
7 am ragi Java
7.30 am prayer
8am classes
9.15 am breakfast
Classes until 1.30
1.30 to 2.30 lunch
2.30 to 4.30 study hour
4.30 to 5 snacks
5.00 to 6 pm walking ,playing
6 to 6.30 prayer
7 pm dinner
Till 9 pm study hour
9pm sleep
In 7th class she started developing symptoms.
After 7th she stopped going to school as it got worse and she was frequently visiting hospitals.
She went to hostel again after her att treatment and subsidence of symptoms in dec.
Was fine until January and she came back home again .
At home :
6am wake up
7 am tea
Breakfast and fruits
Tablets
Sleeps until afternoon
2.30 to 3 lunch
2 months after taking ATT her appetite was increased and she ate more food, frequently- 5times a day
5pm Walking exercises
Eve 6pm fruits
Songs prayers
8pm dinner
9pm sleep
Personal history:
Diet mixed
Appetite normal
bladder movements oliguria
bowel normal
Sleep decreased
Addictions none
Family history
Mother was diagnosed with TB in 2014 and used ATT irregularly.
Symptoms got worse in 2022 and she died in sept 2022
Birth history:
1st born child
Born in 2010
2nd degree consanguineous marriage
Lscs
Father has no idea about immunisation status
Menstrual history
Not attained menarche yet
General examination:
Patient is conscious coherent and cooperative
Well oriented to time place. And person
Patient examined in well lit room
Pallor present
Icterus absent
Cyanosis absent
Clubbing absent
Lymphadenopathy absent
Edema present
Vitals
On 14/3/23
Bp 130/80mmhg
Pulse rate 110 bpm,regular, normal volume
Respiratory rate 32 cpm
Sp02 99%
On 15/3/23
Bp 130/90 mm hg
Respiratory rate 26cpm
Pulse rate 120bpm
Temperature afebrile
Sp02 98%
systemic examination:
Abdominal examination
Shape - slightly distention.
Umbilicus - Inverted
No visible pulsation,peristalsis, dilated veins and localized swellings.
Palpation
soft, tenderness in right and left Hypochondrium, epigastrium.
Percussion
Fluid thrill and shifting dullness present
Auscultation
Bowel sounds heard
No bruit or venous hum.
Respiratory examination
Bilateral air entry present
Dull note
Vocal resonance decreased
Cvs examination
S1 s2 heard, no murmurs
CNS examination
No focal neurological deficits
Higher mental functions normal
Cranial nerves normal
Sensory examination normal sensations
Motor examination normal
Reflexes normal
Investigations
Spot urine sodium 166mmol/l
Spot urinary potassium 20.5
Abg
pH 7.4
Pc02 14.9 mm hg
P02 79.8mm hg
Hc03 9.2 mmol/l
O2 saturation 96%
Serum electrolytes on 14\3
Sodium 136 meq/l
Potassium 4.4 mEq/l
Chloride 106 meq/l
Serum creatinine 0.6mg/dl
Esr 70 mm
CRP neagtive
Blood urea 29 mg\dl
FBS 100 mg\dl
Blood group 0+
Rheumatoid factor negative
HIV non reactive
Hbs ag non reactive
Urine examination:
Colour pale yellow
Appearance clear
Acidic
Specific gravity 1.010
Albumin ++
No sugar, bile salts, bile pigments, rbc, crystals, casts, amorphous deposits
Pus cells 3 to4 \hpf
Epithelial cells 2 to 3 \hpf
On usg
Liver,gallbladder,pancreas,spleen, uterus,ovaries normal
Moderate ascites
Bilateral pleural effusion
Moderate pericardial effusion
Bilateral grade 2 rpd change
Hb 7.5 g\dl
WBC 4200 cells\cumm
Neutrophils 60
Lymphocytes 36
Eosinophils 02
Monocytes 02
Basophils 0
Pcv 24.6 vol%
Mch 76.4 fl
Mchc 30.5%
Rdw 20.6 %
Rbc count 3.2 million\cumm
Platelet 1.57 laksh\cumm
Smear normocytic normochromic anemia
On 15\3
Serum creatinine 1.0 mg\dl
Sodium 1.37 meq\l
Potassium 4.7
Chloride 104
Spot urine protein 393 mg\dl
Spot urine creat 37.8 mg\dl
Ratio 10.3
Clinical images
A 40 year old female patient ,hotel owner, resident of Narketpally came with chief complaints of
- Increased heartbeat since 6 months
- Breathlessness since 6 months
HISTORY OF PRESENT ILLNESS :
Patient was apparently asymptomatic 6 months back then she developed palpitations which were sudden in onset, gradually progressive and develops under stress, heavy work.
It lasts for 2 to 3 min and relives on rest .
Since the last 2 to 3 months she complains of increased frequency and intensity of palpitations.
She also complains of breathlessness ( shortness of breath) since 6 months and it was gradually progressive from grade 1 (6 months back)to 3 (presently)and it relieves on rest.
Patient also has fainting attacks , headache when there is delay in food intake or prolonged standing and it gets relieved on taking rest or food.
PAST HISTORY
Not a known case of Diabetes, Hypertension, Asthma, Tuberculosis,Epilepsy, Thyroid disorders.
Has acidity from past 15 years.
She develops burning sensation in abdomen when she consumes oily food, spicy foods ,chapathi.
And for this she takes pantropazole every morning half n hr before food.
No history of prolonged hospital stay or surgeries.
She had sore throat 2 months back for which she consulted RMP and was given some IV medication and was asked to get thyroid function test and complete blood picture done. Her thyroid profile was normal but her HB was 5.5 gm/dl.(anemic)
RMP gave some oral medications for anemia but she didn't took medication regularly.
TREATMENT HISTORY
Using pantop since 15 years every day morning
FAMILY HISTORY
No relevant family history
MENSTRUAL HISTORY
Menarche at 13 years
Regular cycle , 3/28
Uses 2 pads/day
Not associated with clots
No pain
Has premenstrual symptoms like back pain, leg pain
PERSONAL HISTORY
DAILY ROUTINE
She wakes up at 6.30 am
Does her morning routine
Does household work( sweeping, cleaning dishes,cooking)
Breakfast at 8.30 am
At 9 am she starts preparing items for hotel food, cleans the hotel
Lunch at 2 pm
Tea at 5pm
Dinner at 9 pm
Until then she does hotel work ( cutting vegetables, serves people, cleans hotel, cleans dishes)
Returns to home by 10 or 11 pm
Sleeps by 11 pm
Diet -vegetarian
Appetite- normal
Bowel and bladder movements-regular
Sleep-adequate
Addictions- none
Allergies -none
GENERAL EXAMINATION
Patient was conscious,coherent, cooperative
Built and nourishment- poor
Well oriented to time, place ,person
height- 5.2 inch
Weight-44 kg
BMI- 17.7
Pallor - present
Icterus- absent
Cyanosis -absent
Clubbing-absent
Lymphadenopathy -absent
Edema-absent
VITALS
Temperature -a febrile
BP- 130/90 mmHg
RR- 16cpm
PR- 84bpm
SYSTEMIC EXAMINATION
ABDOMINAL EXAMINATION
Inspection :
Abdomen flat
Moves with respiration
no abdominal distension
umbilicus is central and inverted
no engorged veins
no scars,sinuses,
hernial ornifices are clear
Palpation
All inspectory findings are confirmed
No tenderness
Percussion
No significant findings
Auscultation
Bowel sounds heard
No bruits
RESPIRATORY EXAMINATION
Normal vesicular breath sounds
Trachea central
CARDIOVASCULAR SYSTEM
S1S2 heard
No murmurs
CENTRAL NERVOUS SYSTEM
No focal neurological deficits
Clinical images
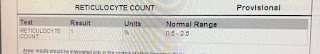
INVESTIGATIONS
FOLATE :3.5ng/ml
IRON : 38 micrograms/dl
TIBC: 453 microgm/dl
%TRANSFERRIN SATURATION : 8%
FERRITIN :12.9 ng/ml
UNSAT IBC : 415.02 microgm/dl
VIT B12 : 223pg/ml
LFT
Ast - 69
Alt- 52
Alp- 176
Tp - 5.9
A/G - 1.45
PROVISIONAL DIAGNOSIS
Dimorphic anemia
Secondary to nutritional cause
?IDA
TREATMENT
Inj Vitcofol 1500MCG IV OD in 100 ml NS
Tab albendazole 400 mg PO OD
Tab Lirogen PO OD every alternate day
Tab esomeprazole 20mg PO OD (7am)
Vitals monitoring every 6th hrly .


































Comments
Post a Comment