Long case
A 62 year old male came to the OPD with chief complaints of
CHIEF COMPLAINTS:
Pedal edema since 1 month
Decreased urine output since 1 month
Fever since 3 days
HISTORY OF PRESENTING ILLNESS:
Patient was apparently asymptomatic 3 years back then developed pedal edema, shortness of breath, fever, cough and was admitted in a private hospital hyd and diagnosed as renal failure.
In February 2022 patient came to kamineni Narketpalli with chief complaints of shortness of breath and decreased appetite and undergone dialysis under 3 sessions and was on conservative management.
In November 2022, patient came with similar complaints and undergone dialysis here
Now he developed pedal edema since 1 month which is pitting type and complained of fever since 3 days which is continuous ,high grade and associated with chills and rigor.
H/o nausea, vomiting, anorexia on 4th jan night.
Vomiting is non projectile, non bilious, non blood tinged contained food particles associated with nausea in 2-3 episodes.
H/o decreased urine output since 1month
No h/o burning micturition, pain abdomen.
H/o abscess over left medial and infra gluteal region 1 year back.
Came for dialysis ( no regular follow up)
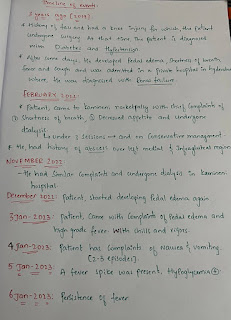
Timeline of events:
PAST HISTORY:
K/C/O Diabetes since 3 years
K/C/O Hypertension since 3 years and on medication for both
Patient had a history of knee injury 3 years back for which he undergone surgery.
N/K/C/O CAD, epilepsy, asthma, Tuberculosis.
No history of any blood transfusions.
FAMILY HISTORY: No significant family history
PERSONAL HISTORY:
DIET: Mixed
APPETITE: Decreased
SLEEP: Adequate
BOWEL MOVEMENTS: Regular
BLADDER MOVEMENTS: Decreased urine output
ADDICTIONS: Drinks toddy occasionally
GENERAL EXAMINATION:
Patient is conscious, coherent and cooperative Well oriented to time, place and person
Moderately built and moderately nourished.
Pallor-absent
Icterus-absent
Cyanosis-absent
Clubbing-absent
Lymphadenopathy-absent
Pedal edema-present
VITALS:. .
Temp:Febrile(102°F)
Blood pressure:130/90mmHg
Pulse rate:82bpm
Respiratory rate:14cpm
SYSTEMIC EXAMINATION.
CVS EXAMINATION :-
JVP: Normal
INSPECTION:
Chest wall symmetrical
Pulsations not seen
PALPATION:
Apical impulse – normal
Pulsations – normal
Thrills absent
PERCUSSION:
No abnormal findings
AUSCULTATION:
S1, S2 heard
No murmurs
No added sounds
RESPIRATORY EXAMINATION :-
- Chest bilaterally symmetrical, all quadrants
moves equally with respiration.
- Trachea central, chest expansion normal.
- Resonant on percussion
- Bilateral equal air entry, no added sounds heard.
1. Breath sounds - Normal Vesicular Breath sounds
2. Added sounds - absent
3. Vocal Resonance - normal
4. Bronchophony, Egophony, Whispering Pectoriloquy absent
No focal neurological deficit.
3) ABDOMINAL EXAMINATION :-
INSPECTION:
1. Shape – flat
2. Flanks – free
3. Umbilicus – Position-central, Shape-normal
4. Skin – normal
5. Hernial Orifices - normal
PALPATION:
Abdomen is soft and non tender
No hepatomegaly
No splenomegaly
No other palpable swellings
Hernial orifices normal
PERCUSSION:
Fluid Thrill/Shifting dullness/Puddle’s sign absent
AUSCULTATION:
Bowel sounds – normal
No bruits, rub or venous hum
PROVISIONAL DIAGNOSIS:
CKD secondary to DIABETIC NEPHROPATHY
With Anemia secondary to CKD
With pyrexia under evaluation ?UTI
INVESTIGATIONS:
◆Hemogram:
Hemoglobin-8.1gm/dl
WBC-7,800 cells/cu mm
Neutrophils- 70%
Lymphocytes- 20%
Eosinophils- 02%
Monocytes- 7%
Basophils- 0
PCV- 25 vol%
MCV- 89.9 fl
MCH- 30.2 pg
MCHC- 31.2 %
RBC count- 2.68 millions/cumm
Platelet counts- 2.09 lakhs/ cu mm
SMEAR:
RBC - normocytic normochromic
WBC - with in normal limits
Platelets - Adequate
Haemoparasites - no
◆Complete urine examination:
Colour - pale yellow
Appearance- clear
Reaction - acidic
Sp.gravity - 1.010
Albumin - trace
Sugar - nil
Bile salts - nil
Bile pigments - nil
Pus cells - 6-8/HPF
Epithelial cells - 2-3/HPF
RBC s - nil
Crystals - nil
Casts - nil
Amorphous deposits - absent
◆Serum creatinine:
5.8 mg/dl
◆Blood sugar: Hypoglycemia:
◆Blood urea:
◆Serum iron:
◆Serum electrolytes:
Sodium - 139 mEq/L
Potassium - 5.0 mEq/L
Chloride - 105 mEq/L
Calcium ionised - 0.90 mmol/L
◆Liver function test:
Total bilirubin - 0.73 mg/dl
Direct bilirubin- 0.19 mg/dl
AST - 17 IU/L
ALT - 10 IU/L
Alkaline phosphatase - 139 IU/L
Total proteins - 5.4 g/dl
Albumin - 3.2g/dl
A/G ratio - 1.51g/dl
◆ECG:
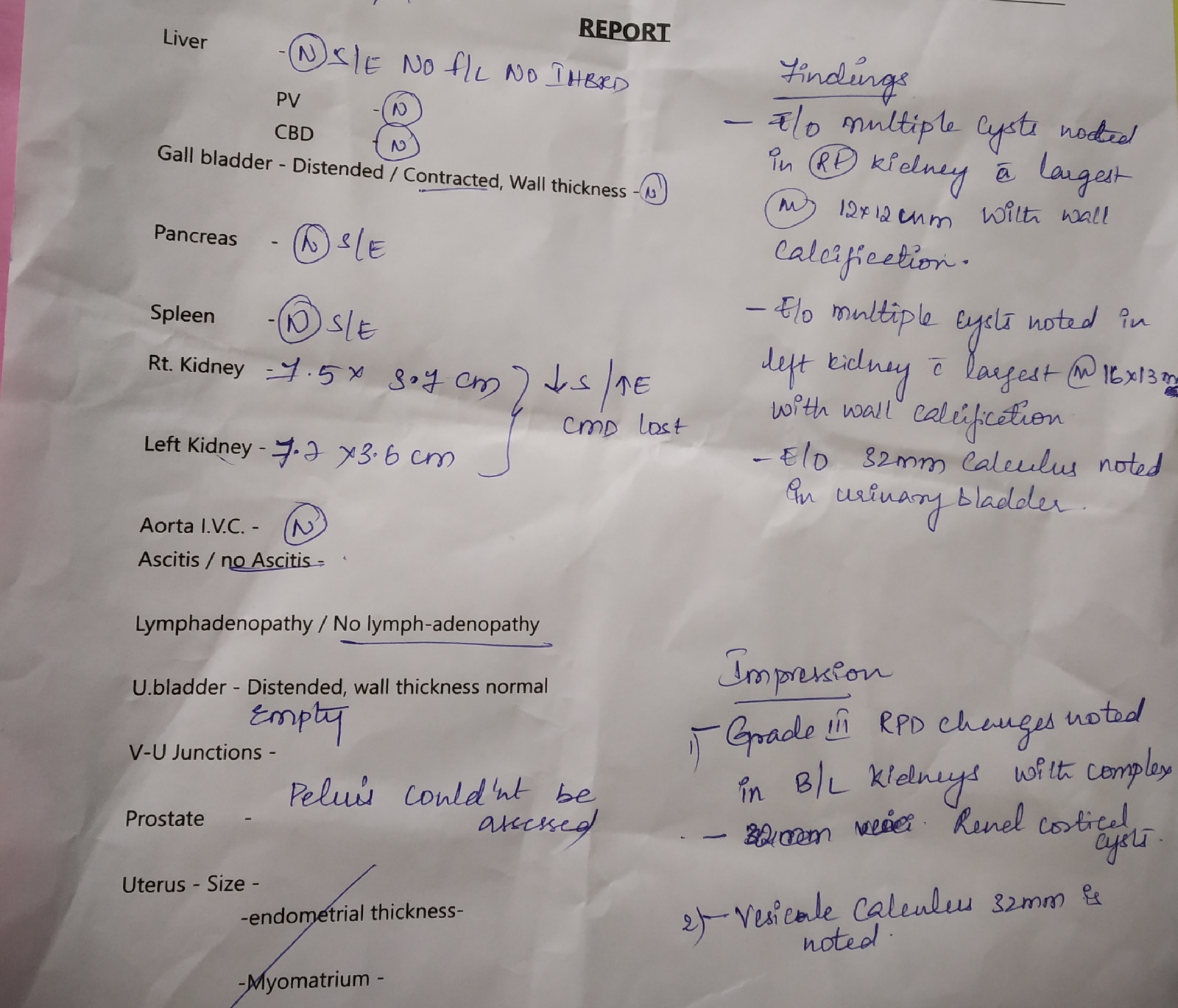
1)Grade lll RPD changes noted in bilateral kidneys with complex renal cortical cysts.
2)Vesicle calculus 32mm is noted.
Doppler studies:
DISCUSSION:
Chronic kidney disease secondary to diabetic nephropathy associated with anemia.
----------------------------------------------------------------------------------------------------------------------------------------------------
SHORT CASE
CHIEF COMPLAINTS:
50 Years old male ,resident of miryalaguda,works in ice factory, came with chief complaints of right sided weakness (upper limb and lower limb) , deviation of mouth to left side and slurring of speech since 2 days (12/3/2023 at 4 am).
HISTORY OF PRESENT ILLNESS:
Patient was apparently asymptomatic 1month back then he developed giddiness and weekness in left lower limb and left upper limb(lowerlimb> upper limb), so he went to the hospital , there he diagnosed with hypertension,they gave antihypertensives (amlodipine and atenolol).his left sided weakness was resolved in 3 days.he took the antihypertensives for 20 days and after that he stopped medications since 10 days onwards because his friends told that take alcohol it will resolves the weakness of limbs. So he stopped medications and took the alcohol since 10 days.on 11/3/2023 night also he took alcohol and slept , on 12/3/2023 at 4am he woke up but he developed giddiness, unable to stand due to weekness in the right upper and lower limbs, deviation of mouth to left side and slurring of speech. So he was taken to the miryalaguda hospital there he underwent CT scan then they referred to our hospital.he came to our hospital on 13/3/2023.
There is no history of difficulty in swallowing, behavioural abnormalities, fainting, sensory disturbances, fever, neck stiffness, altered sensorium, headache, vomiting, seizures, abnormal movements, falls.
DAILY ROUTINE:
Daily he wake up at 4:00am does his morning routine and drinks tea and goes to work ,at 9 '0 clock he comes to home and have breakfast and goes to work till 2 pm and will have his lunch at home ,he then again goes to work till 9pm returns home will have his dinner and sleeps at 10pm.
PAST HISTORY:
Fracture near the right elbow due to fall from the tree 30 years ago ,so he cannot extending his right hand completely.
He is a known case of hypertension since 1 month.
Not a k/c/o Diabetes,asthma, coronary artery diseases,epilepsy,thyroid disorders.
PERSONAL HISTORY:
Diet- mixed
Appetite - normal
Sleep -normal
Bowel and bladder -regular
Addictions-
-He is chronic alcoholic since 30 years, stopped 3 years back but again started 6 mns back after death of his daughter's husband.
-he chews tobacco since 10 years (1 packet per 2 days).
FAMILY HISTORY:
No similar complaints in the family.
TREATMENT HISTORY:
He is on Antihypertensives (amlodipine and atenolol) since 1mn but 10 days onwards he stopped medications.
GENERAL EXAMINATION:-
-Patient is conscious, cooperative, with slurred speech
Well oriented to time, place and person
-Moderately built and moderately nourished.
Vitals :-
Temp - afebrile
BP - 140/80 mm Hg
Pulse rate - 78 bpm
Respiratory rate - 14 cycles per minute
Pallor - absent
Icterus - absent
Cyanosis - absent
Clubbing - absent
Lymphadenopathy - absent
Oedema - absent
SYSTEMIC EXAMINATION:
1) CNS EXAMINATION :-
Dominance - Right handed
Higher mental functions
• conscious
• oriented to time,person and place
• memory - immediate,recent,remote intact
•slurring of speech
Cranial nerves -
I - no alteration in smell
II - no visual disturbances
III, IV, VI - eyes move in all directions
V - sensations of face normal, can chew food normally
VII - Deviation of mouth to the left side, upper half of left side and right side normal VIII - hearing is normal, no vertigo or nystagmus IX,X - no difficulty in swallowing
XI - neck can move in all directions
XII - tongue movements normal, no deviation
Power:-
Rt UL - 3/5 Lt UL-5/5
Rt LL - 3/5 Lt LL-5/5
Tone:-
Rt UL - Increased
Lt UL- Normal
Rt LL- Increased
Lt LL- Normal
Reflexes:
Superficial reflexes:
Right Left
Corneal : present present
Conjunctival: present present
Abdominal: present in all quadrants
Plantar : not elicited flexion
Deep tendon reflexes:
Right Left
Biceps ++ ++
Triceps ++ ++
Supinator ++ ++
Knee jerk +++ ++
Ankle jerk +++ ++
Sensory system -
-Pain, temperature, crude touch, pressure sensations normal
-Fine touch, vibration, proprioception normal
-two point discrimination -able to discriminate and tactile localisation -able to localise
Cerebellum -
Finger nose test normal, no dysdiadochokinesia, Rhomberg test could not be done
RESPIRATORY SYSTEM
Inspection:
Shape of the chest : elliptical
B/L symmetrical ,
Both sides moving equally with respiration
No scars, sinuses, engorged veins, pulsations
Palpation:
Trachea - central
Expansion of chest is equal on both side
Tactile vocal fremitus Normal
Auscultation:
. Normal vesicular breath sounds sounds heard
CARDIOVASCULAR SYSTEM
Inspection :
Shape of chest- elliptical shaped chest.
No engorged veins, scars, visible pulsations
JVP is not raised
Palpation :
Apex beat can be palpable in 5th inter costal space medial to mid clavicular line
No thrills and parasternal heaves can be felt
Auscultation :
S1,S2 are heard
no murmurs
ABDOMEN EXAMINATION:
Inspection -
Umbilicus - inverted
All quadrants moving equally with respiration
No scars, sinuses and engorged veins , visible
pulsations.
Palpation -
soft, non-tender
no palpable spleen and liver
Percussion - liver dullness is heard at 5th intercoastal space
Auscultation- normal bowel sounds heard.
PROVISIONAL DIAGNOSIS:
Right hemiparesis due to cerebrovascular accident probably involving internal capsule.
INVESTIGATIONS :
Anti HCV antibodies rapid - non reactive
HIV 1/2 rapid test - non reactive
Blood sugar random - 109 mg/dl
FASTING BLOOD SUGAR- 114 mg/dl
Hemoglobin- 13.4 gm/dl
WBC-7,800 cells/cu mm
Neutrophils- 70%
Lymphocytes- 21%
Eosinophils- 01%
Monocytes- 8%
Basophils- 0
PCV- 40 vol%
MCV- 89.9 fl
MCH- 30.1 pg
MCHC- 33.5%
RBC count- 4.45 millions/cumm
Platelet counts- 3.01 lakhs/ cu mm
SMEAR:
RBC - normocytic normochromic
WBC - with in normal limits
Platelets - Adequate
Haemoparasites - no
COMPLETE URINE EXAMINATION:
Colour - pale yellow
Appearance- clear
Reaction - acidic
Sp.gravity - 1.010
Albumin - trace
Sugar - nil
Bile salts - nil
Bile pigments - nil
Pus cells - 3-4 /HPF
Epithelial cells - 2-3/HPF
RBC s - nil
Crystals - nil
Casts - nil
Amorphous deposits - absent
LIVER FUNCTION TESTS:
Total bilirubin - 1.71 mg/dl
Direct bilirubin- 0.48 mg/dl
AST - 15 IU/L
ALT - 14 IU/L
Alkaline phosphatase - 149 IU/L
Total proteins - 6.3 g/dl
Albumin - 3.6 g/dl
A/G ratio - 1.36
Blood urea - 19 mg/dl
Serum creatinine - 1.1 mg/dl
Electrolytes:
Sodium - 141 mEq/L
Potassium - 3.7 mEq/L
Chloride - 104 mEq/L
Calcium ionised - 1.02 mmol/L
THYROID FUNCTION TESTS:
T3 - 0.75 ng/ml
T4 - 8 mcg/dl
TSH - 2.18 mIU/ml
ECG
Impression:
Acute infarct in posterior limb of left internal capsule
Old lacunar infarct in left side of pons
Few microhemorrhages in bilateral cerebral hemispheres.
CONFIRMED DIAGNOSIS:
Cerebrovascular accident with Right sided hemiparesis ,
Acute infarct in posterior limb of internal capsule.
TREATMENT:-
Tab. ECOSPRIN
Tab. CLOPITAB
Tab. ATOROVAS
Tab. STAMLO BETA
Physiotherapy




-2.jpg)









Comments
Post a Comment