1801006096 CASE PRESENTATION
LONG CASE
A 50 year old male presented with chief complaints of SOB and pedal edema since 10 days.
History of presenting illness:-
Patient was apparantly asymptomatic 1year back. Then he developed SOB grade 4 which is intermittent and with that he diagnosed with CKD 1 year ago.
Bilateral pedal edema which is pitting type.
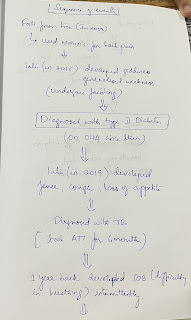
Apparantly asymptomatic 14 years ago,(2008) then he had a history of fall from tree for which he got backpain and then used medication for that.later,8 years ago (2015), he was diagnosed with type-2 diabetes mellitus. History of TB 2years ago and used ATT for 6months.
Seasonal SOB and wheeze on and off since 3 years, with CKD 1 year ago.
Increased SOB and edema since 10 days.
He stopped going to work since last 3 years due to pain and intermittent SOB.

Past history:—
K/c/o TB 2years ago
K/c/o type2 DM since 8 years (on OHA)
K/c/o BP
No H/o Asthma and thyroid.
Personal history:—
Diet- mixed (with non-veg predominant)
Sleep-adequate
Appetite- decreased
Bowel and bladder- decreased urine output.
Addictions- alcohol (daily)stopped 2years ago ,now occasionally
Family history:- not relevant.
General examination:—
Patient is conscious coherent and cooperative,moderately built and nourished.
Pallor-absent
Icterus-absent
Cyanosis-absent
Clubbing-absent
Lymphadenopathy-absent
Pedal edema- seen bilaterally (pitting type)
Vitals:—
Temperature- afebrile
Pulse rate- 103bpm
RR- 35cpm
Blood pressure-150/90 mmhg
Grbs:- 203mg/dl
SpO2:- 97% @room air
Systemic examination:—
Cardiovascular system:-
Inspection:-
Appears normal in shape
Apex beat not visible
No scars , sinuses and dilated veins.
Mild JVP raise.
Palpation:—
All inspectory findings are confirmed
Trachea central in position.
Apex beat- 5th intercoastal space lateral to mid clavicular line.(1cm)
Percussion:-
Heart borders are within normal limits.
Auscultation:—
S1 and S2 heard.
RS:— BAE present
Trachea- centrally located
Shape of chest- bilaterally symmetrical and elliptical.
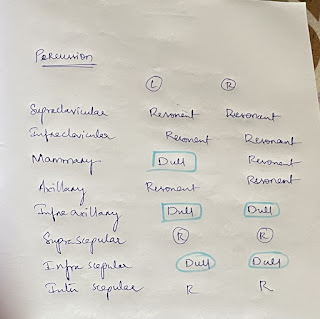
Percussion:—
Dull note heard over left side. (In mammary,infraaxillary and infra scapular regions.)
Little dullness over right side. (In infraaxillary and infrascapular regions.)
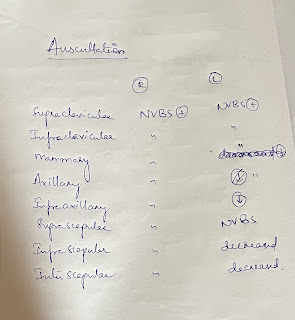
NVBS are less heard in infraaxillary,infrascapular and inter scapular regions.
CNS:—
No abnormal deficits seen.
Bowel sounds heard.
Investigations:—
Hemogram:-
Hb- 11.4g/dl
Total count- 10000 cells /cumm
Neutrophils- 69%
Lymphocytes-18%
Monocytes-11%
Basophils-0
PCV- 35.7
MCV- 83.6
MCH- 26.7
MCHC- 31.9
No hemoparasites seen.
Ultrasound:—
USG CHEST:
IMPRESSION:
BILATERAL PLEURAL EFFUSION (LEFT MORE THAN RIGHT) WITH UNDERLYING COLLAPSE.
2D echo:—
MR +ve, TR +ve (moderate)
Renal function tests:-
Urea- 64mg/dl
Creatinine- 5.9mg/dl
Spot urine protein- 34
Spot urine creatinine- 14.8
Electrolytes-
Na- 139mEq/L
K-3.1 mEq/L
Cl-101mEq/L
Ca- 0.85 mmol/L.
Liver function tests:—
Total bilirubin-0.9mg/dl
Direct bilirubin-0-1mg/dl
Indirect bilirubin-0.8mg/dl
Alkaline phosphatase- 221 u/l
AST-40u/L
ALP- 81u/L
Total protein-6.8g/dl
Albumin-4.2g/dl
Globulin-2.6g/dl
Albumin globulin ratio - 1.6
FBS— 93mg/dl
PLBS- 152mg/dl
ECG:-
ABG:—
PH- 7.3
PCo2- 28.0
PO2- 77.4
HCo3- 13.5
X ray:—
Provisional diagnosis:-
-Heart failure with reduced ejection fraction.
With Acute kidney injury on chronic kidney disease (NSAID induced or diabetes induced).
And bilateral pleural effusion (left side is more than right side)
Treatment:—
-Fluid restriction less than 1.5lts per day.
-salt restriction less than 1.2gm perday
-INJ Lasix 40 mg IV/BD.
-TAB MET XL 25mg PO/OD
-TAB Cinod 5 mg PO/OD.
-INJ human actrapid insulin SC/TID
-INJ PAN 40 mg IV/OD
-INJ ZOFER 4mg IV
- vitals monitoring
-TAB Ecosprin AV 75/10 mg PO/HS.
60 year old female was admitted to opd with chief complaints of
1.Fever since 10 Days
2.Backache since 10days
3.Generalised weakness since 10 days
History of presenting illness:—
Patient was apparently asymptomatic 10 days ago.Then she developed high grade fever which was sudden in onset , continuous without diurnal variation and associated with chills.
She even complained of backache since 10 days which is insidious in onset , gradually progressive and persistent , dull aching and non radiating pain.
She even complained of generalized weakness since 10 days. and devoleped bilateral pedal edema.
Then she went to govt hospital where she was diagnosed with low blood pressure and decreased platelets.
As her condition was not improving she was admitted in our hospital.
Past history:
Not a known case of Diabetes, Hypertension, Asthma ,TB, epilepsy and thyroid disorders.
No history of previous surgeries.
Personal history:
Diet : Mixed
Appetite: decreased
Sleep: disturbed
Bowel and bladder movements : Regular
History of smoking 2 to 3 times a day since 40 yrs (chutta).
Family history:
No significant family history
Treatment history:— antipyretic and antibiotics (unknown).
General examination:
Patient is conscious coherent and cooperative
Moderately built and nourished
Well orientated to time place and person
Pallor - present
Icterus - absent
Cyanosis- absent
Clubbing- absent
Lymphadenopathy - absent
Pedal edema - pesent
Vitals:
Temperature : afebrile
BP: 80/60 mm hg
Pulse: 90 bpm
RR: 30cpm
Systemic examination:
Abdominal examination:
Inspection:
On inspection abdomen is slightly distended, no flank fullness, umbilicus is centre and slit like.No scars seen.No engorged veins
Palpation:
All inspectory findings are confirmed.
Tenderness is seen on the right hypochondrium region.
Percussion:
No significant findings
Auscultation:
Bowel sounds heard
CVS: S1 S2 heard
Respiratory system : Bilateral air entry present Normal vesicular breath sounds heard
CNS: No focal neurological deficits
Investigations:—
Hemogram:—
Hb-10.9
Neutrophils-73
Lymphocytes-25
Monocytes-2
Basophils-0
PCV-33.0
MCV- 87.3
MCH- 28.8
MCHC- 33
RBC count- 3.78 million
Platelet count- 30,000
No hemoparasites found.
Impression:— Normocytic normochromic anemia with thrombocytopenia.
Fever chart:—
Treatment:—
IV fluids-normal saline with 1 ampoule of optineurin
Inj. Noradrenaline 2ampoules in 46ml od normal saline.
Inj PAN 40mg IV
Tab PCM per oral TID
inj . Neomal.























Comments
Post a Comment