1801006097 CASE PRESENTATION
long case
Supra clavicular: normal normal
Infra clavicular: normal normal
Mammary: normal normal
Infra axillary: normal decreased
Supra scapular: normal normal
Infra scapular: normal decreased
Inter scapular: normal normal
Infra clavicular: resonant resonant
Mammary: resonant dull
Axillary: resonant dull
Infra axillary: resonant dull
Supra scapular: resonant resonant
Infra scapular: resonant dull
Inter scapular: resonant dull
Supra clavicular:. Normal normal
Infra clavicular: Normal Normal
Mammary: Normal Normal
Axillary: Normal normal
Infra axillary: Normal decreased
Supra scapular: Normal normal
Infra scapular: Normal decreased
Inter scapular: Normal normal
2D echo
MODERATE MR+: MODERATE TR+ WITH PAH: TRIVIAL ECCENTRIC TR+
GLOBAL HYPOKINETIC, NO AS/MS. SCLEROTIC
MODERATE LV DYSFUNCTION+
DIASTOLIC DYSFUNCTION PRESENT
ULTRASOUND:
USG CHEST:
IMPRESSION:
BILATERAL PLEURAL EFFUSION (RIGHT MORE THAN LEFT) WITH UNDERLYING COLLAPSE.
USG ABDOMEN AND PELVIS:
MILD TO MODERATE ASCITES
RAISED ECHOGENICITY OF BILATERAL KIDNEYS.
X RAY NECK:
DIAGNOSIS:-
HEART FAILURE WITH reduced EJECTION FRACTION
WITH ACUTE KIDNEY INJURY ON CHRONIC KIDNEY DISEASE (SECONDARY TO DIABETES/NSAID INDUCED)
WITH K/C/O DM II SINCE 3 YEARS
WITh TB 3 years ago
Presenting complaints:
A 45 years old male,resident of kodakonla mandal,janagam district hotel server by occupation came with chief complaints of abdominal distension and shortness of breath and swelling of both lower limbs since 1 week.
HOPI: patient was apparently alright 7 days back then he developed swelling in the both limbs which was insidious in onset , gradually progressive,it was pitting in nature, no aggravating and relieving factors
He developed shortness of breath which was insidious in onset , gradually progressive , initially grade 2 but now progressed to grade 3 ,aggravated on walking relieved on taking rest .
Patient was alright 6 years ago and then he developed a minor injury to neck which was not healing and then went for regular checkup and was diagnosed as having diabetes and started on OHA, and 3 years ago he was diagnosed to be having hypertension and started on Tab. Telmisartan 40mg/OD,and was asymptomatic 7 months ago and then in the evening he suddenly became ,unresponsive and irrelevant talk and was taken to hospital and was found to be having hypoglycaemia and was asked to stop OHA,and was found to be having jaundice at that time and was asked to avoid alcohol but he didn’t stopped alcohol consumption.
And 5 months ago,he developed similar complaints and was admitted here and was diagnosed to be having,Acute decomponsated liver disease and was kept on conservative management, a diagnostic and therapeutic tap was done,showing 200cells,lymphocytic predominant cells and High saag and low protein profile and therapeutic Paracentesis was done 1L on day 1
1.75L on day 2 and 1.5L on day 3 and his complaints resolved and was discharged in a hemodynamically stable state,and was normal till 15 days and started developing pedal edema ,abdominal distension and SOB again and came here for further management.
Decreased Apetite and sleep since 2 days.
Chronic alcoholic since 20 years and last binge,30days ago.
Chronic smoker since 30years
Past history:
K/c/o CLD Since 5 months
K/c/o HTN since 2 years
K/c/o DM II since 6 years
Personal history:
Chronic alcoholic consumes 3 quarters/day
Chronic smoker 40 cigarettes/day (since 30 years)
GENERAL PHYSICAL EXAMINATION:
At admission
Patient is drowsy but arousable,
Icterus : present
Clubbing: present
Edema : present ( pedal edema)
No signs of cyanosis, generalised lymphadenopathy
Vitals:
Bp 140/80mmHg
PR 98bpm
RR 18cpm
Temp Afebrile
Spo2 98% on RA
SYSTEMIC EXAMINATION:
CARDIOVASCULAR SYSTEM:
S1 AND S2 HEARD.
NO MURMURS
RESPIRATORY SYSTEM: Bilateral air entry PRESENT.
NVBS HEARD
CENTRAL NERVOUS SYSTEM:
Patient is drowsy and arousable
Speech normal
No signs of meningeal irritation
P/A:
Inspection:
Abdomen is distended , flanks are full
umbilicus everted,
Dilated veins present over the lower aspect of abdomen
No visible scars and sinuses
Palpation:
no local rise of temperature
No tenderness
Fluid thrill absent
Abdominal girth 124cms
Percussion:
Shifting dullness present
Auscultation:
bowel sounds not heard
Provisional diagnosis:
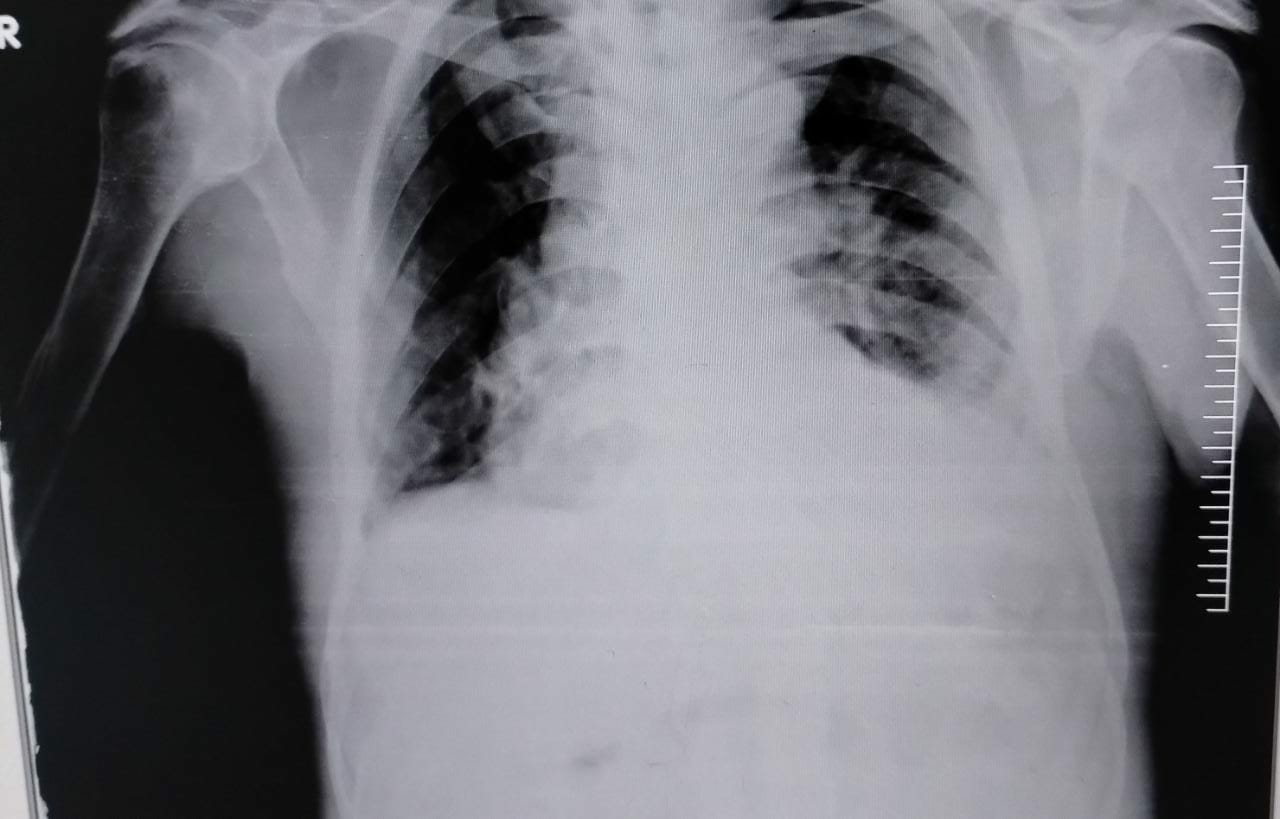
Chest x ray:
APTT: 35 SEC
BLEEDING TIME: 2MIN 30 SEC
CLOTTING TIME: 5 MIN
BLOOD GROUPING: O POSITIVE
BLOOD UREA: 36 mg/dl
SERUM CREATININE: 1.2 mg/dl
PROTHROMBIN TIME: 18 sec
INR: 1.33
HCV: NEGATIVE
HBSAG: NEGATIVE
HIV : NEGATIVE
FBS: 103 mg/dl
SAAG:
SERUM ALBUMIN: 2.2 gm/dl
ASCITIC ALBUMIN: 0.3 gm/dl
SAAG: 1.9
ASCITIC FLUID PROTEIN : 0.8 g/dl
ASCITIC FLUID SUGAR: 151 mg/dl
ASCITIC FLUID AMYLASE: 40.6 IU/L
ASCITIC FLUID LDH: 56.6 IU/L
ASCITIC FLUID ADA: 24 U/L
2D ECHOCARDIOGRAPHY:
No RWMA, MILD LVH (+) (1.2cms)
MODERATE TR+; PAH TRIVIAL AR+; NO MR
SCLEROTIC AV, NO AS/MS
EF: 62. RVSP= 42+10= 52 MM HG
GOOD LV SYSTOLIC FUNCTION
NO DIASTOLIC DYSFUNCTION
MINIMAL PE(+)
IVC SIZE (1.25CMS) COLLAPSING
MILD DILATED R.A/R.V
Blood urea: 16 mg/dl
Serum creatinine: 1.1 mg/dl
Serum Na+ 137 mEq/L
Serum K+ 4.0 mEq/L
Serum Cl- 105 mmol/L
Serum Ca+2 1.05 mmol
Diagnosis:
ACUTE DECOMPENSATED ALCOHOLIC LIVER DISEASE
WITH ASCITIS (MODERATE)
WITH GRADE I HEPATIC ENCEPHALOPATHY
WITH ANEMIA(MACROCYTIC)
WITH K/C/O DM 6 YEARS AND HTN 3 YEARS
TREATMENT:
1. INJ. LASIX 60 mg IV/BD
2. INJ. CEFTRIAXONE 2 GM IV/BD
3. INJ. VITAMIN K 10 mg IV/OD
4. FLUID RESTRICTION less than 1.5 litres/day
5. SALT RESTRICTION less than 2 gm/day
6. INJ. PAN 40 mg IV/PD
7. TAB. ALDACTONE 50mg PO/OD
8. TAB. TELMISARTAN 40 mg PO/OD
9. TAB. RIFAGUT 550 mg PO/BD
10. TAB. UDILIV 300 mg PO/OD
11. SYRUP. HEPAMERZ 15 ml PO/TID
12. O2 inhalation
13. Vitals monitoring
14. Abdominal girth monitoring
15. Grbs monitoring
16. SYRUP. LACTULOSE 30 ml PO/TID
























Comments
Post a Comment