1801006106 CASE PRESENTATION
A 65 years old Man Who is Resident of Narketpally who was Alcohol Seller & Shepherd by Occupation Came with C/O
Fever since 6 months cough since 6 months associated with weight loss , and shortness of breath.
History of presenting illness :
No history of vomiting , loose stools, abdominal pain
Past History:
At 10 years of Age Patient Was apparently Asymptomatic Till 10 years of Age & Once day He Climbed & Fell Down While Cutting Tree leaves for feeding Their Goats & Had a Fracture of Lt.Forearm & Went to Nalgonda District Hospital where Cast was applied & After 20 days He developed infection & a part of Bone was Protruded out & That part of Bone was excised.
10 years Back :
After Having a alcohol Patient Developed Generalized Weakness & Got admitted in Our Hospital for 4-5 days
7 years Back :
Patient Developed Giddiness & Went hospital & was diagnosed with DM2 & HTN for which he was Prescribed Tab.METFORMIN 500mg
6 Months Back :
Patient Developed Both Lower Limb Swelling which was Pitting type & Upto Knees & Diagnosed to have Left Upper Ureter Calculi & CKD For which he was planned for Surgery But Couldn't not be done as patient wasn't fit for Surgery & Was Managed Conservatively with Tab.NODOSIS 500mg BD.
Personal history
Diet : Mixed
Bowel and bladder : Regular
Sleep : Adequate
Family history : not significant
General examination:
Pt is conscious coherent and cooperative well oriented to time place and person
Pallor : Present
Cyanosis : Absent
Clubbing : Absent
Lymphadenopathy : Absent
Temperature : a febrile
Blood pressure : 170/80mmhg
Pulse rate : 130bpm
Respiratory rate : 15cycles per minute
--------------------------------------------------------------------------------------------------------------------------
short case
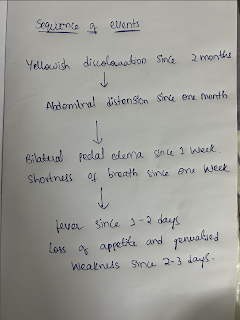
gradually progressive since 3months,associated with h/o yellow discolouration of urine.
B/L pedal edema since 1week ,insidious onset ,gradually progressed till knees,associated with abdominal distension which is present since one month .
• Shortness of breath since 1 week,insidious onset ,gradually progressive
•Fever since 1-2days,High grade not associated with chills,relievedwith medication,which was diffuse,non radiating,no aggregating and relieving factors
• loss off appetite and generalised weakness since 2-3days
N h/ o vomitings
N h/o loose stools , vomitings .
Past history
1 year ago yellowish discolouration of eyes present after which he stopped drinking alcohol for 3 months and later started drinking again
No history of diabetes , hypertension, tb , ASTHMA , epilepsy, CAD
Family history
Not significant
Personal history
Alcoholic since 5 years drinks about 180ml of alcohol per day
•Non smoker
•Bowel bladder habits regular
•Mixed diet
•Sleep adequate
General examination
Patient is conscious,coherent,cooperative , patients is thin built.
Vitals :
PR : 130bpm, regular
Bp: 100/60mmhg
Tempt : 103 F
Spo2 :96% at Room air
•RR:28cpm
•Grbs:128mg/dl
•Jvp normal
Pallor ++
Icterus ++
NO cyanosis , clubbing , lymphadenopathy
pedal edema ++ upto knees , pitting type
Investigations :
RFT :
Urea : 26
Creatinine : 0.8
Sodium : 128
Potassium : 3.0
Hemogram:
Hemoglobin:6.8gm/dl
Total leukocyte count : 13,000cells
Neutrophils : 86%
LFT :
Total bilirubin : 10.20
Direct bilirubin : 4.20
AST : 161
ALT: 72
Total protein : 6.4
Albumin :1.51
Blood culture : no growth
Urine culture : no growth
Serum amylase: 42
Serum lipase : 40
Ascitic fluid :
Cell count : 1570 cells 60% N
Cytology : acute inflammatory smear, negative for malignancy
Protein : 0.7
Sugar: 46
Albumin:0.21
Culture : no growth
Pleura fluid :
Cell count: 2550 70% neutrophils
LDH 641
Total protein : 3.3
Lights criteria : exudative
Culture : no growth
ECG :
Systemic examination :
Per abdomen :
INSPECTION: •Shape:Distended
•Umbilicus:inverted,vertically drawn down
•Skin over the abdomen is shiny
•All quadrants are moving equally with respiration
•No visible peristalsis,Hernial orifices intact
•Visible superficial abdominal vein running vertically down is seen
•External genitalia normal
Palpation:
•Temperature:Not raised
•Tenderness+,diffuse all quadrants
•Rebound tenderness +
•No guarding,rigidity
•Harvey’s sign : flow of blood away from umbilicus above the level of umbilicus and below the level of umbilicus
•No hepatospleenomegaly
Percussion
Shifting dullness +
No fluid thrill
Puddles sign –not elicited
Liver span-12cm
Auscultation
Bowel sounds+
Respiratory system:
Inspection
•Shape of chest:Bilaterally symmetrical,Elliptical in shape
•No visible chest deformities
•No kyphoscoliosis,
•Abdomino thoracic respiration,No irregular respiration
•No tracheal shift
•No dropping of shoulders,Spino scapular distance appears equal on both sides,no sinuses,scars,engorged veins
Palpation:inspectory findings confirmed by Palpation
•Chest movements -normal
Percussion:
Resonant note heard over all areas except infraaxillary and infrascapular
Auscultation: Norma vesicular breath sounds,Decreased breath sounds in B/L infraaxillary,infrascapular areas
Vocal resonance:Decreased in basal areas
Cardiovascular system:
Inspection:precordium normal,apex beat :5th ICS half inch medial to mid clavicular line
Palpation:inspectory findings confirmed,No thrills or parasternal heave
Auscultation: S1S2+,no murmurs
CNS:HMF normal,cranial nerves intact,motor and sensory examination normal
No cerebellar or meningeal signs
Provisional diagnosis :
Ascites secondary to chronic liver disease
Bilateral pleural effusion


















Comments
Post a Comment