1801006108 CASE PRESENTATION
LONG CASE
CHIEF COMPLAINTS:
A 40 Yr old male resident of Krishnapuram, Nalgonda dist, field assistant by occupation presented with the chief complaints of:
- pain abdomen since 6 days
- nausea and vomiting since 6 days
- abdominal distention since 5 days
Patient was apparently asymptomatic 6 days ago, then he developed pain in abdomen of epigastric region which is severe, squeezing type, constant, radiating to the back and aggravated on doing any activity and relieved on sitting and bending forward.
He developed nausea and vomiting which was 10-15 episodes which was non bilious, non projectile and food as content.
and then he developed abdominal distention 5 days ago which is sudden onset, gradually progressive to current state.
no history of decreased urine output, facial puffiness,edema
no history of fever, shortness of breath, cough
PAST HISTORY :
history of diabetes since 5 years
history of hypertension since 5 years
no history of asthma,TB,epilepsy and thyroid disorders.
PERSONAL HISTORY:
Appetite: decreased
Diet: mixed
Sleep: adequate
Bowel and Bladder movements : regular
Addictions: history of alcohol intake for 5 years
DAILY ROUTINE:
He works as a field assistant under NREGS, nalgonda from last 15 years, he supervises around 200-250 workers daily. He goes to his work on his bike at 9 in the morning and comes back home around 5 in the evening.
Since 5 years, the work stress made him to take alcohol with his colleagues from the work and consumes around 60ml of whiskey on a daily basis
5 years ago- started drinking alcohol
↓
3 years ago- admitted in a hospital with the similar complaints, got treated and discharged after 5 days
↓
since 5 days, he couldn't cope up the work stress,consuming alcohol continuously taking around 500 ml daily, skipping food and not going to home
↓
developed pain abdomen and nausea,vomiting
FAMILY HISTORY:
History of diabetes to patient's mother since 14 years
History of diabetes to patient's father since 15 years
TREATMENT HISTORY:
metformin plus glimiperide
telmisartan 40 mg
GENERAL EXAMINATION:
Patient is conscious, coherent, cooperative and well oriented to time,place and person
Adequately built and Adequately nourished
Pallor - Absent
Icterus -Absent
Clubbing - Absent
Cyanosis - Absent
Lymphadenopathy -Absent
Pedal Edema - Absent
Vitals :
Temperature - 99 F
Pulse Rate - 80 beats per minute , Regular Rhythm, Normal In volume, No Radio-Radial or Radio-Femoral Delay
Blood Pressure - 130/90 mmHg measured in the left upper limb, in sitting position.
Respiratory Rate - 13 breaths per minute and regular
SYSTEMIC EXAMINATION:
Patient examined in a well lit room, after taking informed consent.
GASTROINTESTINAL SYSTEM EXAMINATION
Oral Cavity: Normal
Per Abdomen :
Inspection -
Shape - Uniformly Distended
Umbilicus - displaced downwards
Skin - No scars, sinuses, scratch marks, striae, no dilated veins, hernial orifices free, skin over the abdomen is smooth
External genitalia - normal
Palpation -
No local rise in temperature, tenderness in epigastric area
Liver not palpable
Spleen not palpable
Kidneys are not palpable
Abdominal Girth - 84 cm
Xiphisternum - Umbilicus Distance - 21 cm
Umbilicus - Pubic Symphysis Distance - 15 cm
Spino-Umbilical Distance - 19 cm and equal on both sides
Percussion -
Shifting Dullness - Present
Liver dullness at 5th intercoastal space along midclavicular line - Normal
Spleen Percussion - Normal
Tidal Percussion - Absent
Auscultation -
Bowel Sounds - Absent
No Bruit or Venous Hum
CARDIOVASCULAR SYSTEM EXAMINATION
Inspection -
Chest Wall is Symmetrical
Precordial Bulge is not seen
No dilated veins, scars, sinuses
Apical impulse - Not Seen
Jugular Venous Pulse - Not Raised
Palpation -
Apical Impulse - Felt at 5th Intercostal space in the mid clavicular line
No thrills, no dilated veins
Auscultation -
Mitral Area - First and Second Heart Sounds Heard, No other sounds are heard
Tricuspid Area - First and Second Heart Sounds Heard, No other sounds are heard
Pulmonary Area - First and Second Heart Sounds Heard, No other sounds are heard
Aortic Area - First and Second Heart Sounds Heard, No other sounds are heard
Inspection -
Pulmonary Area - First and Second Heart Sounds Heard, No other sounds are heard
Aortic Area - First and Second Heart Sounds Heard, No other sounds are heard
RESPIRATORY SYSTEM EXAMINATION
Inspection -
Chest is symmetrical
Trachea is midline
No retractions
No kyphoscoliosis
No Winging of scapula
No Scars, sinuses, Dilated Veins
All areas move equally and symmetrically with respiration
Palpation -
Trachea is Midline
No tenderness, local rise in temperature
Tactile Vocal Fremitus - Present in all 9 areas
Percussion -
Percussion Right Left
Supra clavicular: resonant resonant
Infra clavicular: resonant resonant
Mammary: resonant resonant
Axillary: resonant resonant
Infra axillary: resonant resonant
Supra scapular: resonant resonant
Infra scapular: resonant resonant
Inter scapular: resonant resonant
Supra clavicular: resonant resonant
Infra clavicular: resonant resonant
Mammary: resonant resonant
Axillary: resonant resonant
Infra axillary: resonant resonant
Supra scapular: resonant resonant
Infra scapular: resonant resonant
Inter scapular: resonant resonant
No tenderness
Auscultation -
Auscultation: Right. Left
Supra clavicular:. NVBS NVBS
Infra clavicular: NVBS NVBS
Mammary: NVBS NVBS
Axillary: NVBS NVBS
Infra axillary: NVBS NVBS
Supra scapular: NVBS NVBS
Infra scapular: NVBS NVBS
Inter scapular: NVBS NVBS
Supra clavicular:. NVBS NVBS
Infra clavicular: NVBS NVBS
Mammary: NVBS NVBS
Axillary: NVBS NVBS
Infra axillary: NVBS NVBS
Supra scapular: NVBS NVBS
Infra scapular: NVBS NVBS
Inter scapular: NVBS NVBS
No added sounds
Vocal Resonance in all 9 areas- normal
CENTRAL NERVOUS SYSTEM EXAMINATION
All Higher Mental Functions are intact
No Gait Abnormalities
No Bladder Abnormalities
Neck Rigidity Absent
PROVISIONAL DIAGNOSIS: Ascites secondary to pancreatitis
INVESTIGATIONS
USG ABDOMEN :
mild to moderate ascites is seenFINAL DIAGNOSIS:
Ascites secondary to Acute Pancreatitis
MANAGEMENT
NPO
IV Fluids - N/S (urine output+30ml/hr)
Inj. PANTOP 40 mg IV BD
Inj. ZOFER 4 mg IV SOS
Inj, PIPTAZ 2.25 mg IV TID
Tab. AMLONG 20 mg PO OD
Tab.LASIX 40 mg BD
GRBS every 4th hourly
Inj TRAMADOL 1 amp IV+100 ml NS IV OD
Inj, HUMAN ACT RAPID according to sugars
Therapeutic paracentesis around 1L
----------------------------------------------------------------------------------------------------------------------------------------------------
Short Case
A 50 year old male came to opd with the
CHIEF COMPLAINTS:
- shortness of breath since 13 days
- edema of lower limbs since 9 days .
- Decreased urine output since 9 days
HISTORY OF PRESENTING ILLNESS:
Patient was apparently asymptomatic 13 days ago then he developed
-Shortness of breath which was insidious in onset and progressed to Grade 4 ,aggrevated on lying down and walking and relieved on taking rest.
- He also developed bilateral pedal edema ,since 9 days which is pitting in nature which is insidious in onset and it is initially Grade 1 and presently progressed upto Grade2 extending till mid thighs
-He also had decreased urine output since 9 days.
No history of chest pain,palpitations,syncope
no history of fever, cough, burning micturition,change in frequency of urine.
PAST HISTORY:
- History of fall from tree 3 years ago
- Diagnosed with Tuberculosis and Diabetes mellitus 3 years ago
- Noticed swelling in both legs and on consultation was diagnosed with Chronic kidney disease 1 year ago.
- Not a known case of Hypertension, thyroid, Asthma, epilepsy in the past
- No history of any surgeries in the past.
- diagnosed with hypertension when he came to the hospital,no prior use of anti hypertensive drugs.
TREATMENT HISTORY:
Drug history:
- NSAIDS intermittently to relieve neck pain
- Antitubercular therapy 3 years ago
- Metformin 500mg three times a day
PERSONAL HISTORY:-
Diet - mixed
Appetite-decreased
Sleep - adequate
Bowel - regular;
Micturition : decreased urinary output since 9 days
Addictions - occasionally alcohol consumption
Cigarette stopped 25 years back before 1 pack per year.
Daily routine:
He is farmer by occupation and used to go to work by waking up at 6 am and breakfast at 7 am ,completes agriculture/field work by afternoon ,takes rest and has dinner at 8 pm ,sleep at 10pm
consumes non vegetarian diet weekly once for lunch
He stayed at home since the fall from tree due to low backache since last 3 years
FAMILY HISTORY:-
no significant family history
ALLERGIC HISTORY:-
no allergies to any kind of drugs or food items
GENERAL EXAMINATION:-
Patient is conscious, coherent, and cooperative
Moderately built and well nourished
No pallor
No icterus
No cyanosis
No clubbing
No lymphadenopathy
Pitting edema seen in both lower limbs extending till mid thigh areas
VITALS:
Temperature - Afebrile
Pulse Rate - 102 bpm
Respiratory Rate - 15cpm
Blood Pressure - 150/90mmg
Sp02 - 97% at Room air
GRBS - 203 mg/dl
CVS EXAMINATION :
INSPECTION:
- shape of chest is normal
- jugular venous pulse is seen
- no precordial bulge is seen
- apical impulse is not well appreciated
- Apex beat is shifted to 6th intercoastal space
- no parasternal heaves
- no thrills
- no dilated veins
- left heart border is not confined to normal limits
- right heart border is with in confined limits
- mitral area, tricuspid area, pulmonary area, aortic area - S1,S2 heard
- no additional sounds are heard
INSPECTION:
Bilateral Air entry Present
Chest is symmetrical
Trachea is midline
No retractions
No kyphoscoliosis
No Winging of scapula
No Scars, sinuses, Dilated Veins
All areas move equally and symmetrically with respirationPALPATION:
Trachea - Midline
Chest is bilaterally symmetrical and elliptical
Percussion Right Left
Supra clavicular: resonant resonant
Infra clavicular: resonant resonant
Mammary: resonant dull
Axillary: resonant dull
Infra axillary: resonant dull
Supra scapular: resonant resonant
Infra scapular: resonant dull
Inter scapular: resonant dull
Auscultation: Right. Left
Supra clavicular:. NVBS NVBS
Infra clavicular: NVBS NVBS
Mammary: NVBS decreased
Axillary: NVBS decreased
Infra axillary: NVBS decreased
Supra scapular: NVBS NVBS
Infra scapular: NVBS decreased
Inter scapular: NVBS decreased
Supra clavicular: resonant resonant
Infra clavicular: resonant resonant
Mammary: resonant dull
Axillary: resonant dull
Infra axillary: resonant dull
Supra scapular: resonant resonant
Infra scapular: resonant dull
Inter scapular: resonant dull
Auscultation: Right. Left
Supra clavicular:. NVBS NVBS
Infra clavicular: NVBS NVBS
Mammary: NVBS decreased
Axillary: NVBS decreased
Infra axillary: NVBS decreased
Supra scapular: NVBS NVBS
Infra scapular: NVBS decreased
Inter scapular: NVBS decreased
PERABDOMEN:
INSPECTION
Abdomen is Mildly distended
Umbilicus is central in position
A visible scar due to injury due to a fall around the umbilicus.
PALPATION -
No Tenderness on superficial palpation.
Abdomen is Mildly distended
Umbilicus is central in position
A visible scar due to injury due to a fall around the umbilicus.
PALPATION -
No Tenderness on superficial palpation.
No local rise in temperature
Liver is Non Tender and not palpable
Spleen is Not palpable
PERCUSSION:Fluid thrill absent
AUSCULTATION- Bowel Sounds Heard
Liver is Non Tender and not palpable
Spleen is Not palpable
PERCUSSION:Fluid thrill absent
AUSCULTATION- Bowel Sounds Heard
CENTRAL NERVOUS SYSTEM EXAMINATION:
HIGHER MENTAL FUNCTIONS:
- Conscious
- Well Orientation to time, place and person
- Speech and language – normal
- Memory – immediate-retention and recall, recent and remote are present
- No delusions, hallucinations
- No Emotional lability
2.CRANIAL NERVES - left Right
Normal normal
3.MOTOR SYSTEM-
Bulk
Inspection normal normal
Palpation normal normal
Measurement
Upper limb – 10cm below acromion ( same on both )
Lower limb 18 cm below tibial tubercle (same on both)
Tone
Upperlimb Normal Normal
Lowerlimb Normal Normal
Power
a. Neck muscles Good Good
b. Upper limbs
i) Shoulder 5/5 5/5
Flexion-Extension
Lateral Rotation-Medial Rotation 5/5 5/5
Abduction -Adduction 5/5 5/5
ii) Elbow
Flexion-Extension 5/5 5/5
iii) Wrist
Dorsi flexion-Palmar flexion 5/5 5/5
Abduction-Adduction 5/5 5/5
Pronation-Supination 5/5 5/5
iv) small muscles of hand Good Good
v) Hand grip Good Good
c. Lower limbs
i) Hip 5/5 5/5
Flexion-Extension
Abduction-Adduction 5/5 5/5
Lateral Rotation-Medial Rotation 5/5 5/5
ii) Knee
Flexion-Extension 5/5 5/5
iii) Ankle
Dorsi flexion-Plantar flexion 5/5 5/5
Inversion-Eversion 5/5 5/5
iv) Small muscles of foot Good Good
REFLEXES
SUPERFICIAL REFLEXES
A.Corneal reflex Present
B.Conjunctival reflex Present
C.Abdominal reflex Present
D.Plantar reflex Present
DEEP REFLEXES
A.Biceps +2 +2
B.Triceps
+2 +2
C.Supinator
+2 +2
D.Knee jerk
+2 +2
E.Ankle jerk
+2 +2
SENSORY SYSTEM - Normal
CEREBELLAR SIGNS- Absent
SIGNS OF MENINGEAL IRRITATION
- neck rigidity absent
- kernigs sign negative
- brudzinski sign negative
PROVISIONAL DIAGNOSIS :Heart failure Renal failure
INVESTIGATIONS:
Complete blood picture
Hemoglobin 11.7 gm/dl
Total count 9,000 cells/cumm
Neutrophils. 74
Lymphocytes 20
Eosinophils 2
Monocytes 4
Basophils 0
Pcv. 36.5 vol
Mcv. 82.8 fl
RDW- CV 19.1 %
RBC COUNT:. 4.4 million/cu/mm
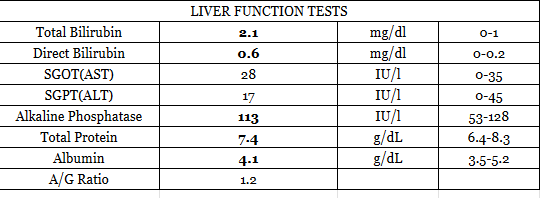
LIVER FUNCTION TEST
Total Bilirubin - 0.9 mg/dl
Direct Bilirubin - 0.1 mg/dl
Indirect Bilirubin - 0.8 mg/dl
Alkaline Phosphatase - 221 u/l
AST - 40 u/l
ALT - 81 u/l
Protein Total - 6.8g/dl
Albumin - 4.2 g/dl
Globulin - 2.6 g/dl
Albumin:Globulin Ratio - 1.6
Renal Function Test
Urea - 64
Creatinine - 4.3
Na+ - 138
K+ - 3.4
Cl- - 104
Fasting Blood Sugar - 93mg/dl
PLBS - 152 mg/dl
HbA1c - 6.5%
ABG :
pH : 7.3
pCO2 - 28.0
pO2 - 77.4
HCO3-.13.5
Spo2-94.7
Total count 9,000 cells/cumm
Neutrophils. 74
Lymphocytes 20
Eosinophils 2
Monocytes 4
Basophils 0
Pcv. 36.5 vol
Mcv. 82.8 fl
RDW- CV 19.1 %
RBC COUNT:. 4.4 million/cu/mm
LIVER FUNCTION TEST
Total Bilirubin - 0.9 mg/dl
Direct Bilirubin - 0.1 mg/dl
Indirect Bilirubin - 0.8 mg/dl
Alkaline Phosphatase - 221 u/l
AST - 40 u/l
ALT - 81 u/l
Protein Total - 6.8g/dl
Albumin - 4.2 g/dl
Globulin - 2.6 g/dl
Albumin:Globulin Ratio - 1.6
Renal Function Test
Urea - 64
Creatinine - 4.3
Na+ - 138
K+ - 3.4
Cl- - 104
Fasting Blood Sugar - 93mg/dl
PLBS - 152 mg/dl
HbA1c - 6.5%
ABG :
pH : 7.3
pCO2 - 28.0
pO2 - 77.4
HCO3-.13.5
Spo2-94.7
2D ECHO:
Aortic Valve - Sclerotic
Moderate MR +, Moderate TR+ with PAH
Global Hypokinetic , No AS/MS
Moderate LV Dysfunction+
Diastolic Dysfunction presentReduced ejection fraction
Aortic Valve - Sclerotic
Moderate MR +, Moderate TR+ with PAH
Global Hypokinetic , No AS/MS
Moderate LV Dysfunction+
Diastolic Dysfunction presentReduced ejection fraction
USG CHEST:
Free fluid noted in bilateral pleural spaces (left more than right)
PROVISIONAL DIAGNOSIS:
HEART FAILURE WITH reduced EJECTION FRACTION
BILATERAL PLEURAL EFFUSION
WITH ACUTE KIDNEY INJURY ON CHRONIC KIDNEY DISEASE (SECONDARY TO DIABETES/NSAID INDUCED)
WITH ACUTE KIDNEY INJURY ON CHRONIC KIDNEY DISEASE (SECONDARY TO DIABETES/NSAID INDUCED)
TREATMENT:
- rest is advised
- Fluid Restriction less than 1.5 Lit/day
- Salt restriction less than 1.2gm/day
- INJ. Lasix 40mg IV / BD
- TAB MET XL 25 mg
- TAB. CINOD 5 MG PO/OD(IF SBP MORE THAN 110 MM HG)
- INJ. HUMAN ACTRAPID INSULIN SC/TID (ACCORDING TO SLIDING SCALE)
- INJ. PAN 40 MG IV/OD
- INJ. ZOFER 4 MG IV/SOS
- Strict I/O Charting
- Vitals Monitoring
- TAB. ECOSPRIN AV 75/10 MG PO/OD
















Comments
Post a Comment