1801006136 CASE PRESENTATION
long case
CHIEF COMPLAINTS
- Abdominal Distention since 1 month
- Decreased appetite since 20 days
No History of Vomiting
No History of Diarrhea or Constipation
No History of Burning Micturation
No History of Hemoptysis
DAILY ROUTINE
Pulmonary Area - First and Second Heart Sounds Heard, No other sounds are heard
Aortic Area - First and Second Heart Sounds Heard, No other sounds are heard
Inspection -
Supra clavicular: resonant resonant
Infra clavicular: resonant resonant
Mammary: resonant resonant
Axillary: resonant resonant
Infra axillary: resonant resonant
Supra scapular: resonant resonant
Infra scapular: resonant resonant
Inter scapular: resonant resonant
Supra clavicular:. NVBS NVBS
Infra clavicular: NVBS NVBS
Mammary: NVBS NVBS
Axillary: NVBS NVBS
Infra axillary: NVBS NVBS
Supra scapular: NVBS NVBS
Infra scapular: NVBS NVBS
Inter scapular: NVBS NVBS


ULTRASOUND ABDOMEN
- Coarse echotexture of Liver - CLD?
- Cholelithiasis
- Moderate Loculated Ascites with septations
----------------------------------------------------------------------------------------------------------------------------------------------------
short case
CHIEF COMPLAINTS
A 28 year old female who is a housewife, resident of Miryalguda, came to the OPD with chief complaints of :
- Cough since 1 week
- Shortness of Breath since 1 week
HISTORY OF PRESENTING ILLNESS:
Patient was apparently asymptomatic 1 week back. Then she developed cough since 1 week which was insidious in onset, gradually progressive, non productive, and aggravated at night.No known relieving factors
She also complained of breathlessness since 1 week which was insidious in onset, gradually progressive from mMRC grade II to grade III, associated with wheeze, palpitations, sweating and Orthopnoea.
C/o chest pain which was dragging type, non radiating on the left side associated with chest tightness, no aggravating or relieving factors .
H/o fever 1 week back, subsided with medication.
On the day of examination the patient complained of productive cough.
There is no h/o loss of appetite, reduced urine output or loss of weight
PAST HISTORY:
No similar complaints in the past
No h/o inhaler usage
No past h/o TB
N/K/C/O HTN, DM, Epilepsy, CAD, asthma
H/o 2 previous LSCS.
PERSONAL HISTORY:
Build and Nourishment : Moderately built, Well Nourished.
Diet: Mixed
Appetite: Normal
Bowel and Bladder: regular
Sleep - Disturbed since last 1 week, was adequate before
No addictions
No known allergies to drugs or food
Daily Routine:
6 AM - Wake up, does morning routine, household chores
9 AM - Prepares breakfast, sends children to school, and husband to work
10 AM - 12 PM - Watches TV
1230 PM - 1 PM - Prepares and has Lunch
2 PM - 4 PM - Takes a nap
4 PM - Socialises with neighbours
5 PM - Children and husband return home, has some tea and snacks
6 PM - 7 PM - Spends time with family
8 PM - Prepares Dinner
9 PM - 10 PM - Has dinner and watches TV
10 PM - Goes to bed
FAMILY HISTORY:
No history of similar complaints in the family
MENSTRUAL HISTORY:
Age of menarche: 12 years.
Cycle: 3/28
Not associated with pain or clots
LMP: 1/12/22
OBSTETRIC HISTORY:
Age of marriage: 18 years
Age at first child birth: 22 yrs
Para: 2
Number of living children:3
Birth history: LSCS
GENERAL EXAMINATION:
The patient is conscious, coherent, cooperative, and well oriented to time, place and person.
No pallor, icterus, cyanosis, clubbing, koilonychia, lymphadenopathy or edema
No malnutrition or dehydration
VITALS:
Temp: Afebrile
PR: 126 bpm
BP: 130/90 mm Hg
RR: 38 cpm
SPO2: 98% @ RA
SYSTEMIC EXAMINATION:
Patient is examined in a well lit room and in a sitting position.
Upper Respiratory Tract:
Nose: No DNS, polyps, turbinate hypertrophy
Oral cavity: No ulcers
Lower Respiratory Tract:
INSPECTION:
Shape of chest: elliptical
Trachea: appears to be central
Supraclavicular and infraclavicular hollowness absent
Accessory muscles usage - None
Apical impulse Normal
No kyphoscoliosis
No hyperpigmented patches, scars
PALPATION:
All inspectory finding confirmed
Trachea: central
Tactile vocal fremitus: Not assessed
Chest movements: not assessed
PERCUSSION:
Direct: resonant
Indirect: Right Left
Supra clavicular:. Resonant Hyperresonant
Infra clavicular: Resonant Hyperresonant
Mammary: Resonant Hyperresonant
Inframammary Resonant Dull
Axillary: Resonant Hyperresonant
Infra axillary: Resonant Dull
Supra scapular: Resonant Hyperresonant
Infra scapular: Resonant Dull
Inter scapular: Resonant Hyperresonant
AUSCULTATION: Right Left
Supra clavicular:. NVBS NVBS
Infra clavicular: NVBS NVBS
Mammary: NVBS NVBS
Inframammary NVBS Diminished
Axillary: NVBS NVBS
Infra axillary: NVBS Diminished
Supra scapular: NVBS NVBS
Infra scapular: NVBS Diminished
Inter scapular: NVBS NVBS
Tricuspid Area - First and Second Heart Sounds Heard, No other sounds are heard
Pulmonary Area - First and Second Heart Sounds Heard, No other sounds are heard
Aortic Area - First and Second Heart Sounds Heard, No other sounds are heard
PER ABDOMEN:
INSPECTION: Not Distended
PALPATION: Inspectory Findings Confirmed
Soft, non tender
No Organomegaly
PERCUSSION : Tympanic
AUSCULTATION: Bowel sounds Heard
CNS:
No focal neurological deficits
Cranial Nerves intact.
PROVISIONAL DIAGNOSIS:
Left sided HYDRO PNEUMOTHORAX
INVESTIGATIONS:
CT - CHEST
Large non homogenous opacities with air bronchogram and surrounding ground glass opacities is seen in the superior segment of the left lower lobe
LIGHTS CRITERIA
- fluid protein/serum protein = 0.22
- fluid LDH/serum LDH = 2.28
- 2/3 of upper limit of serum LDH = 306<513
Exudative Effusion
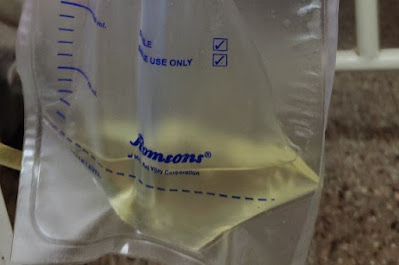
ICD inserted:
Tube: patent
Drain: 200ml
Air column: 3-4cm
Air leak +
Subcutaneous emphysema - Absent
Post procedure vitals:
PR: 128bpm
BP: 120/70mmhg
RR: 36cpm
SPO2: 99% with 12-14 liters/min of oxygen
TREATMENT:
1.O2 inhalation @ 2-3l/min to maintain saturation >94%
2. Inj PIPTAZ 4.5mg IV/TID
3. Inj PAN 40 mg IV/OD/BBF
4. Inj TRAMADOL 1 amp in 100ml NS stat
5. Syrup GRILLINCTUS-DX 2tsp TID
6. Inj ZOFER 4mg IV/STAT
7. T. DOLO 650mg PO BD
8. Monitor vitals- BP, PR, RR, SPO2
9. ICD care:
- Bag always below waist
- Cap always open
- Check air column movement
- Maintain under water seal.
11. Tab. AZEE 500mg PO OD
FINAL DIAGNOSIS: LEFT SIDED HYDRO-PNEUMOTHORAX SECONDARY TO INFECTION















Comments
Post a Comment