1801006145 CASE PRESENTATION
long case
A 50 year old male presented with chief complaints of SOB and pedal edema since 10 days.
HISTORY OF PRESENTING ILLNESS:-
The patient was apparently asymptomatic till 2008; then he fell down from a tree while working in the field and he developed Backache which was persistent and relieved on rest (he did not use any medication for a year). After a year he used started using medication ( painkillers as said by the patient drug unknown; dose unknown; which relieved his pain but he stopped going to work.
In 2015; the patient started having shortness of breath grade 2 and a high fever with chills and rigor, relieved by taking medication.
There was a history of dizziness and he was taken to a local government hospital where he was investigated and found to have
DM - type 2 for which he was prescribed Metformin( dose - 500mg; no side effects are seen due to drugs) and he used them regularly with regular diet management and mild exercise.
Then after 3 years in 2019; he developed a fever with night sweats; chills; cough which contains sputum (color unknown); loss of appetite; loss of weight; then he was taken to a higher center where a sputum examination was done and was diagnosed with TUBERCULOSIS; and he was started on ATT which he used for 6 months regularly and after that, he was tested again and got negative.
After 3 Years in May 2022, there was a minor accident with a fire and then he noticed that there was swelling in both legs he was investigated to see creatinine of 3.5 and diagnosed with CKD and was started on some medication ( drug unknown)
But the swelling subsided for some days.
From then on he intermittently has pedal edema and shortness of breath.
In 2023 Jan he developed shortness of breath grade 3 and was rushed to a hospital, and said to have a heart; lung, and kidney abnormalities; and was admitted to the hospital for 2 weeks, where they gave him some medication, but did not use properly after on and symptoms persisted.
10 days back he had sudden onset of shortness of breath which is GRADE IV,
Edema of both upper and lower limbs For 6 days
Lower limb edema which is pitting type (grade 4 ) up to the thigh.
In a private hospital And was referred to our hospital for further management
Past history:—
DM since 6 yrs ( metformin is used 500 mg)
TB 3 yrs ago .
No history of thyroid, hypertension, asthma
No history of any surgeries in the past.
Drug history:- intermittent use of NSAIDS for the past 14 years
Personal history:—
Diet- mixed (with non-veg predominant)
Sleep-adequate
Appetite- decreased
Bowel and bladder- decreased urine output.
Addictions- alcohol (daily)stopped 2years ago, now occasionally
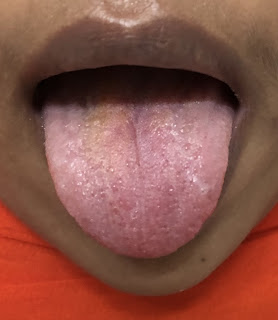
General examination:—
Patient is conscious coherent and cooperative,moderately built and nourished
Pallor-absent
Icterus-absent
Cyanosis-absent
Clubbing-absent
Lymphadenopathy-absent
Pedal edema- seen bilaterally (pitting type)
Vitals:—
Systemic examination:—
Respiratory system :
BAE present
Trachea- centrally located
Shape of chest- bilaterally symmetrical and elliptical.
Percussion:—
Auscultation :
NVBS are less heard in infraaxillary,infrascapular and inter scapular regions.
CNS:-
The patient is conscious.
No focal deformities.
cranial nerves - intact
sensory system - intact
motor system - intact
Per abdomen:- soft non tender
Bowel sounds heard.
Investigations:—
Hemogram:-
Hb- 11.4g/dl
Total count- 10000 cells /cumm
Neutrophils- 69%
Lymphocytes-18%
Monocytes-11%
Basophils-0
PCV- 35.7
MCV- 83.6
MCH- 26.7
MCHC- 31.9
No hemoparasites seen.
Ultrasound:—
USG CHEST:
IMPRESSION:
BILATERAL PLEURAL EFFUSION (LEFT MORE THAN RIGHT ) WITH UNDERLYING COLLAPSE.
2D echo:—
MR +ve, TR +ve (moderate)
Renal function tests:-
Urea-191mg/dl
Creatinine- 5.9mg/dl
Spot urine protein- 34
Spot urine creatinine- 14.8
Electrolytes-
Na- 139mEq/L
K-3.1 mEq/L
Cl-101mEq/L
Ca- 0.85 mmol/L.
Liver function tests:—
Total bilirubin-0.9mg/dl
Direct bilirubin-0-1mg/dl
Indirect bilirubin-0.8mg/dl
Alkaline phosphatase- 221 u/l
AST-40u/L
ALP- 81u/L
Total protein-6.8g/dl
Albumin-4.2g/dl
Globulin-2.6g/dl
Albumin globulin ratio - 1.6
FBS— 93mg/dl
PLBS- 152mg/dl
ECG :
ABG:—
PH- 7.3
PCo2- 28.0
PO2- 77.4
HCo3- 13.5
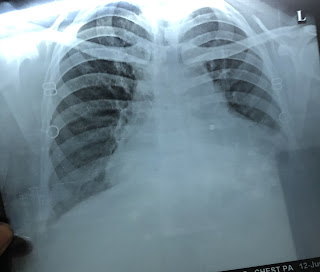
Chest xray:—
Provisional diagnosis:-
-Heart failure,
With Acute kidney injury on chronic kidney disease
And bilateral pleural effusion (left side is more than right side)
Treatment:—
-Fluid restriction less than 1.5lts per day.
-salt restriction less than 1.2gm perday
-INJ Lasix 40 mg IV/BD.
-TAB MET XL 25mg PO/OD
-TAB Cinod 5 mg PO/OD.
-INJ human actrapid insulin SC/TID
-INJ PAN 40 mg IV/OD
-INJ ZOFER 4mg IV
- vitals monitoring
-TAB Ecosprin AV 75/10 mg PO/HS.
----------------------------------------------------------------------------------------------------------------------------------------------------
short case
CVS:
- S1,S2 are heard
- Decreased heart sounds
CNS:
The patient is conscious.
No focal deformities.
cranial nerves - intact
sensory system - intact
motor system - intact




















Comments
Post a Comment