long case
70 year old male came from rural telangana came to opd with chief complaints of decreased urine output from past 16 days.
HOPI:-
Patient was apparently asymptomatic 15 days back later he noticed that there is decrease in his urine output. It is associated with burning micturition. There is no history of pyuria, dysuria, pain abdomen, loin pain.
Reddish discolouration of urine is present 1 days back
Past history:-
The patient gives history of haemodialysis about 10years ago after he had fever with abdominal distension .
He has hypertension from past 10 years initially he was on T.LOSAR H and now presently on T.TELMA H PO OD.
There is no h/o DM, Asthma, Epilepsy, CAD, Thyroid disorders.
Personal history:-
Appetite :- normal
Diet :- mixed
Bowel:- regular
Sleep :- adequate
Addictions:-
Regular alcoholic stopped 12 yra ago.
Regular smoker used to smoke 2to 3 beedis per day stopped 12 years ago.
General examination:-
Patient is conscious coherent and cooperative
No pallor, icterus, cyanosis, clubbing, lymphadenopathy, pedal edema.
Temperature:- 98.5F
BP:- 170/110 mmHg
PR:- 92bpm
RR:- 24cpm
SpO2 :- 99%
CVS :- S1, S2 heared, no murmurs.
PA :- soft and non tender.
CNS:- NFND.
RESPIRATORY SYSTEM EXAMINATION:-
Upper respiratory tract:-
Nose:- ala nasi septum normal
No polyps
Oral cavity normal
Examination of the chest proper :-
Inspection:-
Chest is symmetrical
Trachea is central
No retractions
No winging of scapula
No scars, sinuses , dilated veins
Chest movements decreased on right side of chest ( lower side ) .
Palpation:-
Trachea central
No tenderness, no local raise of temperature
Expansion of chest : not symmetrical decreased on right side.
Tactile vocal fremitus:- decreased on right side infra scapular region.
Percussion.:-
Percussion. Right. Left
Supraclavicular. Resonant. Resonant
Infraclavicular. Resonant. Resonant
mammary. Dull dull
Axillary. Resonant. Resonant
Infraaxillary. Resonant resonant
Suprascapular. Resonant. Resonant
Infrascapular. Resonant. Resonant
Interscapular. Resonant
Auscultation:-
Normal vesicular breathsounds heard in all areas
No added sounds
Vocal resonance decreased in right sided sided infra scapular scapular region
Provisional diagnosis:- Acute kidney injury with pleural effusion.
Investigations:-
Haemoglobin- 9.4g/dl
Lymphocytes- 12%
PCV- 27.9
MCV- 76.0
MCH- 25.6
RBC COUNT- 3.67
Normocytic normochromic anemia.
Blood urea:- 55mg/dl
Serum creatinine:- 1.8mg/dl
Urine protein and creatinine ratio:- 0.53
USG abdomen report:-
Grade 3 prostatomegaly.
Chest x-ray:-
There is obliteration of costophrenic angle on the right side- pleural effusion.
USG chest findings:-
Left ling is normal
Right lung :- moderate pleural effusion noted in the right lung with air bronchograms and collapse of the lower zones.
At 7pm on 16.3.2023 under strict aseptic conditions, under USG guidance, 2% lognocaine was instilled and 20cc syringe was placed in 6th intercostal space in Right interscapular area and 20ml straw colour fluid was aspirated.
Plerural fluid cytology:-
Microscopic findings
Cytosmear studies shows predominantely lymphocytes , few degenerated neutrophils and mesothelial cells against eosinophilic proteinaceous background .No E/o atypical cells
Impression:- negative for mallignancy.
Blood urea:- 23mg/dl
Serum creatinine:- 1.3mg/dl
Sodium:- 136mEq/L
Potassium:- 4.2mEq/L
Chloride:- 104mEq/L
FINAL DIAGNOSIS:- Acute kidney injury with pleural effusion
TREATMENT
1. IV fluids @ 75ml/hr
2. Tab. Urimax D PO
3.tab. cinod 10mg P9 bd
4.tab. silocap d po od
5.syp. citralaka 15ml in one glass of water po tid
6.syp. lactulose 15ml po
----------------------------------------------------------------------------------------------------------------------------------------------------
short case
A 14 year old female , resident of Nagarjuna sagar came to opd with chief complaint of pain in both the lower limb since 7days
HISTORY OF PRESENT ILLNESS
She is second born child of parents married of 3rd degree consanguinity in 2009. All trimesters were uneventful. She was delivered through Cesarean section because of delayed labour pain with birth weight of 3kg.
Immunized till date.
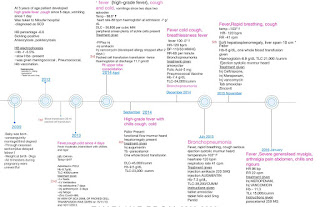
2012
She was asymptomatic up to age of 3 years, then she developed high grade fever with cough and vomiting. She was diagnosed with Sickle cell anaemia. Sickling test positive and Electrophoresis showed HbS. Blood transfusion were given 1packet.
2013
She developed high grade fever, dry cough and cold. She was diagnosed with Bronchopneumonia. X-ray lower lobe consolidation.
2015
She had recurrent episodes of fever, cough , cold i.e. Recurrent Bronchopneumonia- 6 episodes in 3years. Urine culture showed Klebsiella growth.
Blood transfusion till date 4 times.
2016
She developed fever, pain abdomen , myalgia and arthralgia. She improved on medications and thus was discharged.
2019
She came with stomach pain and vomiting. She was diagnosed with Acute pancreatitis.
2023 Jan
Blood Transfusion done
Diagnosed to have cholelithiasis
2023 March
She was apparently asymptomatic 7 days back then she developed pain in left ankle for w8hich she took TAB.ULTRACET and since 4day she developed pain in both knee and then she developed tenderness in the calf muscles it is of throbbing type in nature
She complaints of right lower leg pain from knee to ankle, dragging type, continuous, not relieved on medication associated with swelling below right knee over shin of tibia
She has fever
All the peripheral pulses are palpable
No history of chest pain, shortness of breath, palpitations.
No history epigastric pain, vomiting
No history of headache, seizures, altered mental status
PAST HISTORY
She is a known case of sickle cell anemia
History of bronchopneumonia
History of 8 PICU admissions
History of blood transfusion (20 times till now) last transfusion was done in Jan 2023
No History of asthma, thyroid, Tuberculosis, Hypertension, Diabetes, Epilepsy
No history of bone pain with localized swelling in past
No history of any surgery.
PERSONAL HISTORY
Diet-mixed
Appetite-normal
Sleep-adequate
Bowel and bladder movements are regular
No allergies
No addictions
Not attained menarche
FAMILY HISTORY
3rd degree consanguineous marriage
No known affected relatives
PEDIGREE CHART
IMMUNIZATION HISTORY
patient is vaccinated according to national immunization schedule
Pneumococcal, typhoid, hepatitis vaccine taken on 23/1/22
GENERAL EXAMINATION
Patient was conscious, coherent and cooperative. Well oriented to time, place and person.
Pallor present
Icterus present
Right eye
Local edema on shin of right tibia
No Cyanosis, clubbing, lymphadenopathy
Vitals
Temp: Afebrile
PR- 96 bpm
RR- 18/Min
Bp-110/70mm of hg
Spo2-99%
BP- 110/70 mmHg
Height-144cm
Weight- 36kg
Fever chart
SYSTEMIC EXAMINATION
Per Abdomen - Soft , tender over left hypochondriac. No organomegaly
CVS- S1 and S2 heard ,no murmurs
RS- Bilateral air entry present, normal vesicular breath sounds are heard
CNS-no neurological deficit
PROVISIONAL DIAGNOSIS
Sickle cell anemia with vaso occlusive crisis
INVESTIGATIONS
Hemoglobin- 8gm/dl
TLC-22,900
PCV-23.1(normal- 36 to 46)
BLOOD group -O positive
Total bilirubin-20.15
Direct bilirubin-14.13
SGOT-170
SGPT-180
ALP-560
CRP-negative
Serology -negative
LDH-
blood urea- 20mg/dl
Creatinine-0.4
Electrtrolytes-sodium- 136 mEq/l
Pottasium-4.5 mEq/l
Chloride-101mEq/l
Calcium 1.02mmol/l
Peripheral smear-
Anisopoikilocytosis with predominant Sickle cell, normocytes, few microcytes
WBC count increased
Platelet count increased
Treatment History
IV FLUID IONS @75ml/kg
TAB PENICILLIN 800mg PO
TAB FOLIC ACID 5mg PO OD
TAB ECOSPIRIN 75 mg PO OD
TAB HYDROXYUREA 1000mg PO OD
TAB TRAMADOL 1Ampoule in 100 ml NS SOS
TAB PANTOP 40 mg IV OD
TAB SHELCAL 500mg PO OD
TAB ZOFER 4mg IV SOS
TAB NAPROXEN 250 mg PO BD
















Comments
Post a Comment