Long Case
A 35 yr old male came to opd with chief complaints :
yellowish discoloration of eyes since 15 days ,
abdominal distenstion since 15 days
bilateral swelling of legs since 15 days ,
shortness of breath since 10 days .
HISTORY OF PRESENTING ILLNESS :
patient was apparently asymptomatic 15 days back then he developed abdominal distenstion which is insidious in onset and gradually progressive since 15 days and he has bilateral lowerlimb swelling below knee since 15 days .patient is having breathlessness for 10 days for regular household activities like using toilet, while brushing , walking within home , patient is having itching over all the body since 10 days .
patient has loss of appetite apetite since 1 week .
NO history of abdominal pain.
NO history of chest pain , palpitations, orthopnea
NO history of cough , hemoptysis .
No histroy of melena , hemetemesis .
NO history of epigastric and retrosternal burning sensation .
No history of facial puffiness , burning micturition, decreased urine output .
NO history of confusion , drowsiness.
No history of diarrhoea.
PAST HISTORY:
patient has similar complaints in the past 5 months back and he developed yellowish discoloration of eyes for 3days ,fever was high grade , continuous not associated with chills and rigor , no evening rise of temperature, he went to hospital for 1 week and symptoms subsided after a week following which he continued consuming alcohol since then (180ml per day)
NOT a known case of diabetes, hypertension, asthma , TB , CAD.
PERSONAL HISTORY:
Diet :Mixed
Appetite : decreased
Sleep :normal
Bowel and bladder : constipation is present
Addictions: patient consuming alcohol 180 ml per day since 5 yrs. Non smoker.
FAMILY HISTORY:
NO similar complaints in the family.
GENERAL EXAMINATION:
patient is conscious,coherent, cooperative and well oriented to time ,place and person moderately built and nourished.
Pallor: absent
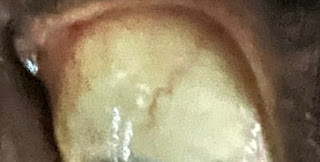
Icterus: PRESENT
cyanosis :absent
clubbing : absent
Edema : Bliateral pitting type of pedal edema is present.
lymphadenopathy:absent


VITALS:
Temperature: 98.4*C
pulse rate: 95 bpm
Respiratory rate :22cpm
SpO2: 98%
GRBS :120 mg/dl
STSTEMIC EXAMINATION
PER ABDOMEN:
INSPECTION:
Abdomen is distended.
flanks are full.
umbilicus is slit like.
skin is stretched , dilated veins present,no visible peristalsis, equal symmetrical movements in all quadrants with respiration.
Peripheral signs of chronic liver disease:
Spider naevi is absent
Palmar erythema is absent
Dupuytrens contracture is absent
Clubbing is absent
Bruises absent
Gynaecomastia absent
fetor hepaticus absent
PALPATION :
No local rise of temperature, no tenderness
All inspectory findings are confirmed by palpation, no rebound tenderness, guarding and rigidity .
No tenderness, spleen palpable in left hypochondrium.
No organomegaly
PERCUSSION-Fluid thrill present
Shifting dullness - absent
AUSCULTATION: Bowel sounds are present .
No bruits .
CVS :
INSPECTION:
chest is symmetrical, no dialated veins , scars and sinuses seen
PALPATION: Apical impulse felt at left 5th inter coastal space medial to mid clavicular line
AUSCULTATION: S1 ,S2 heard no murmurs .
RESPIRATORY SYSTEM:
INSPECTION:
chest is symmetrical, trachea is central
PALPATION:
Trachea is normal
Bilateral chest movements are equal
PERCUSSION:
Resonant in all 9 areas
All quadrants are moving equally
AUSCULTATION:
Normal vesicular breath sounds heard.
CENTRAL NERVOUS SYSTEM:
Higher mental functions - normal memory intact
cranial nerves :Normal
sensory examination:
Normal sensations felt in all dermatomes
motor examination-
Normal tone in upper and lower limb
Normal power in upper and lower limb
Normal gait
Normal reflexes elicited- biceps, triceps, knee and ankle reflexes elicited
cerebellar function-Normal function.
INVESTIGATIONS :
Hemogram -
Hb- 13.2gm/dl
Total leucocyte count - 5000cells /cumm
Neutrophils - 71%
Lymphocytes -22%
RBC - 4.8 million /cumm
Electrolytes-
Sodium- 138mEq/l
Potassium - 4.4mEq/l
Chloride- 104mEq/l
Liver function tests -
Total bilirubin - 4.75mg/dl
Direct bilirubin - 2.11mg/dl
SGOT(AST) - 178 IU/L
SGPT(ALT) - 50 IU/L
ALP- 255IU/L
Total protein - 6.2 gm /dl
Albumin - 2.01 gm/dl
A:G ratio - 0.48
Ascitic tap
Appearance - clear , straw coloured
SAAG - 1.79 g/dl
Serum albumin - 2.01 g/dl
Asctic albumin - 0.22 g/dl
Ascitic fluid sugar - 166mg/dl
Ascitic fluid protein - 2.1 g/dl
Ascitic fluid amylase - 20.8 IU /L
LDH : 150IU/L
Cell count- 150 cells
Lymphocytes 90%
Neutrophils 10%
PT - 15 seconds
INR - 1.4
aPTT - prolonged
CUE:Appearance - clear
Albumin - trace
Sugars - nil
Pus cells - 2to 4
Epithelial cells - 1 to 3
RBC - nil
RFT :Blood urea - 20mg/dl
Creatinine - 0.9mg/dl
PT - 15 seconds
INR - 1.4
aPTT - prolonged
X-RAY:
USG :
Impression- liver normal size
Altered echotexture with surface irregularities present suggestive of chronic liver disease.
Mild spleenomegaly.
DIAGNOSIS
Alcoholic cirrhosis with portal hypertension.
Decompensated features are jaundice and ascites .
currently no hepatic encephalopathy or hepatorenal syndrome .
TREATMENT PLAN:
1. Fluid restriction
2. Salt restricted normal diet
3. Inj.VITAMIN K 1 ampoule in 100 ml NS OD
4. Inj.THIAMINE 1amp in 100ml NS OD
5. Inj.PAN 40mg BD
6.Inj.ZOFER 4mgTID.
7.Syrup LACTULOSE 15ml 30 mins before food TID.
8. Tab. Aldactone 50mg OD
9. Tab. LASIX 40mg BD.
----------------------------------------------------------------------------------------------------------------------------------------------------
short case
55 year male patient farmer by occupation presented with cheif complaints of:
- Slurring of speech since 10 days
-deviation of mouth towards left side since 10days
HISTORY OF PRESENTING ILLNESS
Patient was apparently asymptomatic 10 days ago then he developed slurring of speech and deviation of mouth towards left side which were sudden in onset non progressive and no loss of sensation over limbs and face.Patient is has no complaints at night and sleeps peacefully.WAKES up in the morning with complains of stroke facing difficulty in speaking (he is able to talk but opposite person couldnot understand) difficulty in eating .
No h/o trauma
No h/o drooling of saliva
No h/o difficulty of combing hair,mixing food, squatting,climbing stairs, rolling in bed,lifting up neck.
No h/o of upper and lower limb weakness.
No h/o blurring of vision.
No h/o loss of consiousness.
No h/o altered sensorium.
PAST HISTORY
Patient is a known case of hypertension since 1 year.History of perforation to the tympanic membrane 15 years ago.History of tuberculosis 21 years ago and took medication for 6 months.
PERSONAL HISTORY
Patient takes mixed diet,appetite is decreased,bowel and bladder movements are normal.Addictions : Patient has NO addictions at present,but 20 years ago he used to consume TODDY.No known allergies
DAILY HISTORY
He wakes up at 5 am and does his routine work and have his break fast at 8 am goes to work.He will Have his lunch at 1 -2 pm.He reaches home at around 8 pm has dinner and goes to sleep.
FAMILY HISTORY
Father was a known case of Diabetes ,Hypertension and Tuberculosis and he passed away due to COVID.Mother passed away due to breast cancer.Both the sons of the patient were also affected with tuberculosis at the same time.Both his sisters are known case of diabetes and Hypertension.Brother , sister in law,and both their children were affected with tuberculosis.Brother had history of stroke 3 years back.
GENERAL EXAMINATION
Patient is consious ,coherent ,cooperative and well oriented to time place and person.He is well built and well nourished.
pallor - absent
icterus - absent
cyanosis - absent
clubbing - absent
lymphadenopathy - absent
edema - absent
VITALS
Pulse rate-60 bpm
Respiratory rate- 18 cpm
Blood pressure- 130/80mmHg
Temperature- afebrile
On examination of head to foot, there no presence of neurocutaneous markers,congestive cardiac failure.
SYSTEMIC EXAMINATION
CENTRAL NERVOUS SYSTEM EXAMINATION
Higher mental function-conciousness,oriented to time place and person.
SPEECH - slurring of speech present, no fluency
Memory - Normal,No delusions or hallucinations
CRANIAL NERVE EXAMINATION :-
I- Olfactory nerve-sense of smell is present
II- Optic nerve-direct and indirect light reflex is present
III- Oculomotor nerve IV- Trochlear nerve and VI- Abducens- direct and consenual light reflex, accomodation reflex are present, no diplopia, no nystagmus, no ptosis.
V- Trigeminal nerve
Sensory: sensation present over face.
Motor-Masseter,temporalis and pterygoid muscles are normal.
Reflex- Corneal reflex, conjunctival reflex and jaw jerk is present.
VII- Facial nerve-loss of nasolabial fold on right side and mouth deviated to left side.
VIII- Vestibulocochlear nerve- decreased hearing of the left ear
(rinner’s negative for 256 Hz and 512 Hz) and normal hearing of the right ear.
No nystagmus
IX- Glossopharyngeal nerve- palatal movements present and equal.gag reflex present
X- Vagus- palatal movements present and equal
XI- Accessory nerve- trapezius, sternocleidomastoid contraction present
XII- HYPOGLOSSAL NERVE - DEVIATION OF TONGUE TOWARDS RIGHT SIDE
MOTOR SYSTEM
1) Bulk right left
-appearnace normal normal
-palpation normal normal
-measurements
Upper limb -(arm) 29cm 29cm
(Fore arm) 26cm 25 cm
Lower limb-( thigh) 49cm 49 cm
Leg) 31 cm 31 cm
2) Tone-
Upper limb- normal normal
Lower limb- normal. normal
3) Power-
Upper limb-
Shoulder 5/5 5/5
Elbow 5/5 5/5
Wrist 5/5 5/5
Lower limb-
Hip 5/5 5/5
Knee 5/5 5/5
Ankle 5/5 5/5
Leg 5/5 5/5
4) Reflex:
Biceps reflex 2+ 2+
Triceps reflex 2+ 2+
Knee reflex 2+ 2+
Ankle reflex
Plantar flexion flexion
SENSORY SYSTEM-
Crude touch -present
Pain - present
Temperature- present
Fine touch- present
Tactile localisation-present
2 point discrimination-present
CEREBELLAR SYSTEM-
NO gait ataxia
Nystagmus-no
Dysarthria-present
Intention tremor-absent
Limb coordination tests:
Finger nose test, heel shin test are normal.
dysdiadochokinesis
MENINGEAL SIGNS-
No neck stiffnes,no kernigs and brudzinsky sign
CARDIOVASCULAR SYSTEM EXAMINATION
INSPECTION-chest wall appears normal in shape and symmetrical,no visible pulsations,scars,dilated veins.
PALPATION- apical impulse felt at 5 ICS .
AUSCULATION-s1 s2 heard nor murmurs heard
RESPIRATORY SYSTEM-
INSPECTION -chest wall normal shape and symmetrical movement with repiration, no dilated veins,no scars
PALPATION- trachea central,Chest wall movements symmetrical, tactile vocal fremitus symmetrical.
PERCUSSION - resonant,no pain and tenderness
AUSCULTATION -normal vesicular breath sounds heard ,no addent sounds.
ABDOMEN EXAMINATION
INSPECTION - abdomen round ,umbilicus in center not everted,no visble sinuses and scar,no visible peristalsis,
PALPITATIONS -no pain and tenderness no organomegaly
AUSCULTATION -bowel sounds heard
PROVISIONAL DIAGNOSIS
Sudden onset ,left sided dense hemiplegia with left upper motor neuron facial palsy due Acute cerebrovascular accident involving lenticulostriate branch of left mca territory probably due to thrombus and patient has a risk factor of hypertension
INVESTIGATIONS
Complete blood picture
Hemoglobin:11.7mg/dl
Peripheral smear: normocytic normochromic anemia
Red blood cells:3.86
Pcv:34.6
Platelet count:2.10
Total leucocyte count:5,100
Fasting blood sugar : 92 mg/dl
Serum creatinine :1.3 mg/dl
Blood urea 38 mg/dl
CUE:
Colour : pale yellow
Appearance : clear
Reaction :acidic
Albumin:nil
Sugar: nil
Bile salts and bile pigments : nil
RBC : nil
Crystals :nil
Casts : nil
pus cells:2-3
epithelial cells-2-3
Serum electrolytes
Sodium: 145 mEq/L
Potassium:4.2mEq/L
Chloride:104 mEq/L
Calcium ionized:1.11 mmol/L
CAROTID DOPPLER

MRI REPORT
Infarcts in left internal capsule
TREATMENT
TAB.CLOPITAB 75mg
TAB. Ecospirin 75mg



















Comments
Post a Comment