1801006199 CASE PRESENTATION
long case
A 50 year old male presented to the casualty with weakness of right upper and lower limbs since the morning of 13/3/23 4am. With slurring of speech and deviation of mouth to the left side.
History of presenting illness
Patient was apparently asymptomatic 1 month back, he later developed giddiness followed by a fall. He was diagnosed with hypertension( HTN) to which he used medication for 20 days and stopped 10 days ago.
He was asymptomatic until yesterday when he noticed weakness in his right upper and lower limbs while going to the washroom. It was associated with deviation of the mouth to left side and slurring of speech. Symptoms were sudden in onset and quick in progression.
There is history of (H/O) trauma
There is no H/O difficulty in swallowing, giddiness, headaches, nausea, vomiting, drug intake, chest pain, drug intake, tingling sensation of effected limbs.
Past history
Diagnosed with HTN one month back.
H/O past trauma
No H/O diabetes mellitus, epilepsy, tuberculosis, coronary artery disease, thyroidal illness, HIV, malignancy, fever, drug intake
No previous hospital admissions
Personal history
Diet- mixed
Appetite- normal
Bowel and bladder- regular
Sleep- adequate
Addictions- consumes alcohol( average of 90ml per day)
Family history- no relevant family history
General examination
Consent of the patient was taken
Patient is conscious, coherent and cooperative
Well built and nourished
pallor: absent
Icterus: absent
Cyanosis: absent
Clubbing:absent
Lymphadenopathy: absent
Edema: absent
Temperature: 98°F
Pulse:60 beats/ minute
Blood pressure: 140/80mmHg
Respiratory rate: 14 cycles/minute
No involuntary movements
No abnormal neck swellings
No neck stiffness present
Systemic examination
CENTRAL NERVOUS SYSTEM
*Higher mental functions
Patient is conscious
Oriented to time place and person
Well dressed, well behaved and in a good mood
Speech slightly slurred, language understandable
Memory: intact
*Cranial nerves
Olfactory nerve: smells perceived
Optic nerve: counting fingers 6m
III, IV, VI: ocular motility normal, pupillary reflexes normal
Trigeminal nerve: jaw jerk present, corneal reflexes present
Facial nerve: mouth deviated to the left side
Vestibulocochlear nerve: normal sensory hearing
IX, X: no difficulty in swallowing
Accessory nerve: neck movements normal
*Motor system
No muscle wasting
Normal muscle tone
Power: upper limbs- right 3/5. Left-5/5
Lower limbs- right 3/5. Left- 5/5
Reflexes. Right. Left
Supinator- 3. 5
Biceps. 3. 5
Triceps. 3. 5
Knee. 3. 5
Ankle . 3 5
Coordination
Finger to nose- normal
Dysdiadochokinesia- normal
Knee to hell- normal
Sensation- pain, temperature, proprioception, vibration felt equally on both sides
Gait- unable to walk without support, dragging the right leg
Romberg's test- couldn’t be elicited
CARDIOVASCULAR SYSTEM.
*Inspection- normal shape, bilaterally symmetrical, no percardial bulge, no engorged veins
*palpation- apical beat felt at 5th inter coastal space, no additional pulsation felt, no thrills felt
*percussion- heart borders noted
*auscultation- S1 and S2 heard. No additional heart murmurs
ABDOMEN
*inspection- flat abdomen with no distension, no engorged veins visible, skin over abdomen normal, umbilicus central, hernial orifices normal, external genital normal.
*palpation- no tenderness present, temperature to touch normal, no abnormal swellings.
*percussion- tympanic sound with dullness over solid organs
*auscultation- bowel sounds heard.
RESPIRATORY SYSTEM
*inspection-chest normal shape and bilaterally symmetrical
*palpation-trachea midline, chest movements symmetrical, tactile and vocal fremitus felt
*percussion- no dullness present bilaterally
*auscultation: Normal vesicular breath sounds heard, no added sounds.
Diagnosis: Cerebrovascular accident with right hemiparesis most probably involving left internal capsule
Investigations:
Haemogram:
Haemoglibin 13.4
Total lecucocyte count 7,800
Red blood cells 4.45
Platelets- 3.01
Complete urine examination
Pale yellow clear
Acidic
Trace albumins
Pus cells 3-4
Epithelial cells 2-3
Sugars nil
Thyroid function tests
T3 0.75
T4 8
TSH 2.18
Renal function test
Urea: 19mg/dl
Serum. Creatinine: 1.1mg/dl
S. Na+: 141 mEq/L
S. K+:. 3.7 mEq/L
S. Cl-: 1.02 mmol/L
FASTING BLOOD SUGAR: 114mg/dl
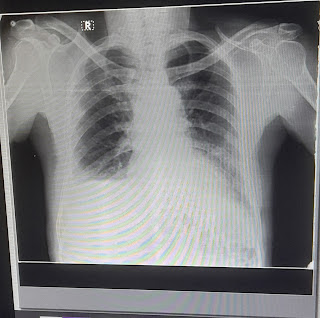
Chest X-ray PA view:
MRI Brain:
Final diagnosis:
1. TAB. ECOSPRIN 150 MG PO/STAT
2. TAB. CLOPITAB 150 MG PO/STAT
3. TAB. ATORVAS 80 MG PO/STAT
4. PHYSIOTHERAPY OF UPPER AND LOWER LIMB
5. I/O CHARTING
----------------------------------------------------------------------------------------------------------------------------------------------------
short case
70 yr old male farmer has presented to the OPD with c/o decreased urine output since 19 days
HOPI
Patient was apparently asymptomatic 19 days ago then he noticed that his urine output has been decreasing. It is associated with burning micturition. No H/o Pyuria, dysuria ,pain abdomen, loin pain.
Reddish discolouration of Urine present 4days back
He also Complains of an Episode of Non bilious vomiting 4days back
The patient also reports that 6 days ago he had an episode of dizziness for which he went to a local hospital where he was diagnosed as BPPV and was managed conservatively.
Past History
The patient gives History of Haemodialysis About 10 yrs ago after He had fever with abdominal distension
He is a K/c/O CVA 15 yrs ago
K/c/o HTN Since 10 yrs initially on T. LOSAR H AND PRESENTLY ON T.TELMA H PO OD
Not a K/c/o DM , Asthma, TB, Epilepsy, CAD , Thyroid disorders
Personal History
Appetite :- Normal
Diet ,:Mixed
Bowel : regular
Sleep :- Adequate
Addictions :-
Regular Alcoholic stopped 12 yrs ago
Regular smoker - Used to smoke 2-3 beedis per day
Stopped 12 yrs ago
General Examination
Patient is C/c/C
No pallor, icterus, cyanosis, Lymphadenopathy, Pedal edema
Temp :- 98.5F
Bp :- 170/110mmHg
PR:- 92 bpm
Spo2 :- 99 % @RA
Systemic examination:
CVS :- S1s2+ No murmurs
RS :- BAE+ NVBS +
PA:- Soft NT
CNS :- NFND
Haemogram: hb: 9.4mg/dl
lymphopenia, PCV decreased, mch, mcv, RBC count decreased
Blood urea: 55mg/dl (normal= 17-50mg/dl)
Serum Creatinine: 1.8 mg/dl (normal = 0.8-1.3mg/dl)
Serum electrolytes:
Sodium: 122mg/dl (normal = 136-145mEq/l
chloride: 90mg/dl (normal = 98-107mEq/l
Spot urine sample:
Urine protein: 8mg/dl
Urine creatinine: 15mg/dl
Ratio : 0.53
ECG:
Chest X-ray PA view:
USG abdomen and pelvis:
Grade 3 prostatomegaly
Rt kidney grade 2 rpd changes
Lt kidney grade 1 rpd changes
Moderate rt side pleural effusion and collapse of rt lower lobe
USG Chest:
Lt lung normal
Rt lung shows moderate pleural effusion with air bronchogram and collapse of lower zones
Diagnosis: Post renal Acute kidney injury due to protatomegaly and right sided pleural effusion
Pleural fluid examination:
Under aseptic conditions under USG guidance and 2% lignocaine instilled and 20cc syringe placed in 6th intercostal space in rt interscapular area and 20ml straw colored fluid is aspirated
Pleural fluid LDH: 486IU/L (normal:230-460IU/L)
Pleural sugar: 80mg/dl (normal: 60-90mg/dl)
Pleural protein: 4g/dl (normal: 0-2.5mg/dl)
pleural fluid cytology:
cytosmear shows predominantly lymphocytes and no malignant cells














Comments
Post a Comment