long case
A 42 YEAR OLD MALE CAME TO OPD WITH
CHIEF COMPLAINTS
- bilateral lower limb swelling since 15 days
-shortness of breath since 2 days
HISTORY OF PRESENTING ILLNESS
-patient was apparently asymptomatic 15 days back then he noticed bilateral lower limb swelling which was insidious in onset gradually progressing pitting type extending up to knee
-later developed shortness of breath since 2 days which was initially grade 2 progressed to grade 4 associated with orthopnea and paroxysmal nocturnal dyspnea
no h/o cough , chest pain
no h/o decreased urine output
no h/o fever, abdominal discomfort
HISTORY OF PAST ILLNESS
no history of similar complaints in the past
no history of diabetes , hypertension , asthma , cardiovascular disease , epilepsy , cerebrovascular accident
PERSONAL HISTORY
Diet - mixed
Appetite - decreased
sleep - decreased
bladder and bowel movements - regular
he has been consuming alcohol 180 ml daily since 20 years
chronic smoker 2 pack beedi / day since past 20 years
FAMILY HISTORY
NO family history of similar complaints
no family history of hypertension and diabetes
GENERAL EXAMINATION
patient is conscious ,coherent, cooperative
thin built and moderately nourished
icterus present
no pallor , cyanosis , clubbing , lymphadenopathy
Jvp raised
VITALS
1. temperature - 98.6f
2. pulse rate - 110 beats per minute regular
3.respiratory rate - 18 cycles per minute
4. blood pressure - 120/80 mmhg
SYSTEMIC EXAMINATION
A. CARDIOVASCULAR EXAMINATION
INSPECTION
chest is barrel shaped , bilaterally symmetrical
trachea is central
movements are equal bilaterally
JVP raised
no scars , sinuses
apical impulse seen in left 6th intercoastal space lateral to midclavicular line
VISIBLE APEX BEAT
Raised jvp
PALPATION
- All inspectory findings are confirmed
apex beat felt in left 6th intercoastal space lateral to midclavicular line
AUSCULTATION
-s1,s2 heard
- no abnormal murmurs heard
RESPIRATORY SYSTEM
INSPECTION
- chest barrel shaped chest, bilaterally symmetrical
-trachea central
-movements are equal bilaterally
-no scars or sinuses
PALPATION
-All inspectary findings are confirmed trachea is central , chest movements are equal bilaterally
- anteroposterior diameter of chest is equal to transverse diameter
AP diameter -23 cm , transverse diameter - 23 cm
-vocal fremitus decreased in infra axillary area and infra scapular area
PERCUSSION
AUSCULTATION
-bilateral air entry present - normal vesicular breath sounds are heard
-breath sounds decreased in right infra axillary area and infra scapular area
-expiratory wheeze heard bilaterally
PER ABDOMEN:
PALPATION
•Shape of abdomen is scaphoid
•no visible epigastric pulsations
•No engorged veins/scars/sinuses
PALPATION
•Soft , non tender
•No organomegaly
•Tympanic node heard all over the abdomen
•Bowel sounds present
CENTRAL NERVOUS SYSTEM:
•Higher motor functions are - Intact •Speech – Normal
•No Signs of Meningeal irritation
•Motor and sensory system – Normal
•Reflexes – Normal
•Cranial Nerves – Intact
•Gait – Normal
•Cerebellum – Normal
•GCS Score – 15/15
PROVISIONAL DIAGNOSIS :
HEART FAILURE
RIGHT SIDED PLEURAL EFFUSION
COPD
INVESTIGATIONS
Chest xray
Showing loss of costophrenic angle and cardiophrenic angle on right side And loss of cardiophrenic angle on left side
LIVER FUNCTION TEST
Total bilirubin 2.6mg/dl (0-1)
Direct bilirubin -1.35 mg/dl (0-0.2)
Sgot-75IU/L (0-35)
Sgpt - 31IU/L (0-45)
Alkaline phospatase -157 IU/L (53-128)
Total protiens 6.1 g/dl
Albumin 3.5
SERUM CREATININE - 2.1 mg/dl (0.9-1.3)
BLOOD UREA -81mg/dl (12-42)
SERUM ELECTROLYTES
sodium -129 meq/l (136-145)
Pottasium -4.8meq/l (3.5-5.5)
Chloride -94meq/l (98-108)
2D ECHO
DIAGNOSIS
HEART FAILURE WITH REDUCED EJECTION FRACTION
Bilateral pleural effusion (right more than left)
TREATMENT
1) Fluid restriction less than 1 litre per day
2) Salt restriction less than 2 grams per day
3) TAB lasix 40 mg bd
4) TAB MET- XL 25mg bd
5) TAB ECOSPIRIN-AV 75/2 mg od
6) BP PR temperature and spo2 monitering
----------------------------------------------------------------------------------------------------------------------------------------------------
short case
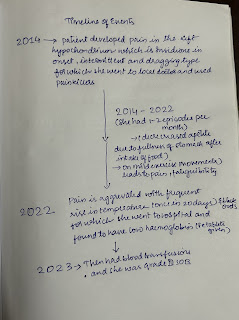
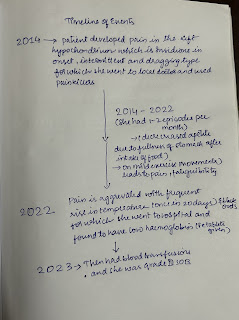
A 23 YEAR OLD FEMALE CAME TO OPD
CHIEF COMPLAINTS
- Left abdominal pain since 1 year
HISTORY OF PRESENTING ILL NESS
- Patient was apparently asymptomatic 9 years back then she started developing pain in left hypochondrium which is insidious in onset intermittent & dragging type. since last one year she is having 1-2episodes of pain every month lasting for 30-60 min.
•c/o frequent onset of fever (once in 15-20 days) since 1 year, for which she visited a local hospital and found to be having low hemoglobin & started oral iron (used for one month) for which she had black colored stools.
•c/o shortness of breath since one year ( Grade III)
•c/o early fatigability, tingling in upper and lower limbs
•decreased appetite since 14 years of age
•No H/o chest pain, pedal edema
•No H/o orthopnea, PND
•No H/o cold , cough
•No bleeding manifestations
•No c/o weight loss
PAST HISTORY
•Not a known case of Hypertension , Diabetes mellitus , Tuberculosis , asthma , thyroid disorders, epilepsy , CVD , CAD
• No H/o surgeries in the past
PERSONAL HISTORY
• Diet - mixed
• appetite - decreased
• sleep - inadequate due to pain
• bowel and bladder - regular
• No addictions and no known allergies
MENSTRUAL HISTORY
age of menarche - 12 yrs
• Regular cycles , 3/28 , changes 3-4 pads per day.
• No gynecological problems
FAMILY HISTORY
no similar complaint in the past
pedigree chart

GENERAL PHYSICAL EXAMINATION
• patient is conscious, coherent, cooperative and well oriented to time, place and person.
• Thin built
• No pallor, icterus, cyanosis, clubbing, lymphadenopathy ,edema.
frontal bossing
VITALS
Temperature : afebrile
Respiratory Rate:18 cycles per minute
Pulse rate : 78 bpm
Blood pressure :110/70 mmHg
SYSTEMIC EXAMINATION
PER ABDOMEN :
• inspection
Shape - flat , no distention
Umbilicus - inverted, round scar around umbilicus
No visible pulsations ,peristalsis, dilated veins
Visible swelling in the left hypochondrium , 6cm×4cm in size, oval shape, smooth, skin over swelling is normal
• Palpation
No local rise of temperature and tenderness
Spleen palpable ( moderate splenomegaly) 5cm below it's costal margin by
CLASSICAL METHOD
No palpable liver
•Percussion
liver span -12 cm
Spleen - dullness extending to umbilical region
Fluid thrill and shifting dullness absent
Auscultation
Bowel sounds: present
CARDIOVASCULAR SYSTEM:
•Inspection
Shape of chest- elliptical shaped chest
No engorged veins, scars, visible pulsations
•Palpation
Apex beat can be palpable in 5th inter costal space medial to mid clavicular line
No thrills and parasternal heaves can be felt
•Auscultation
S1,S2 are heard
no murmurs
RESPIRATORY SYSTEM:
•Inspection
Shape of the chest : elliptical
B/L symmetrical ,
Both sides moving equally with respiration
No scars, sinuses, engorged veins, pulsations
•Palpation
Trachea - central
Expansion of chest is symmetrical.
•Auscultation
B/L air entry present . Normal vesicular breath sounds
CNS:
•HIGHER MENTAL FUNCTIONS- Normal Memory intact
•CRANIAL NERVES :Normal
•SENSORY EXAMINATION
Normal sensations felt in all dermatomes
•MOTOR EXAMINATION
Normal tone in upper and lower limb
Normal power in upper and lower limb
Normal gait
•REFLEXES
Normal
•CEREBELLAR FUNCTION
Normal function
No meningeal signs were elicited
•Provisional diagnosis:-
Splenomegaly with Anemia
INVESTIGATION
HAEMOGLOBIN- 8.7 gm/dl
TOTAL COUNT - 2130 cells/cum
pcv - 30.0
MCV - 789
MCHC - 28.6
peripheral smear- Anisocytosis with normocytes microcytes tear drops pencil forms and macrocytes
impressions -Pancytopenia
APTT Result- 41s
BLOOD UREA- 26 mg/dl
BLEEDING AND CLOTING TIME
bleeding time - 2min
clotting time -4min
BLOOD GROUPING AND RH TYPE-B positive
PROTHROMBIN TIME- 2.0sec
ECG
Usg
Moderate splenomegaly
Portal and splenic vein appears dilated
Bone marrow biopsy
Hypocellular marrow with micronormoblastic maturation of erythroid series
TREATMENT
Livogen -Z tab
Ultracet tab
















Comments
Post a Comment